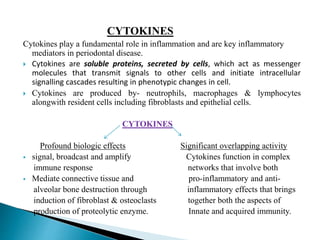
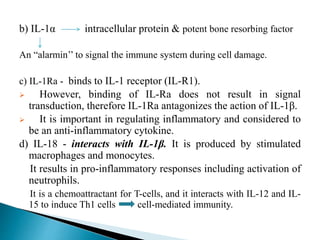
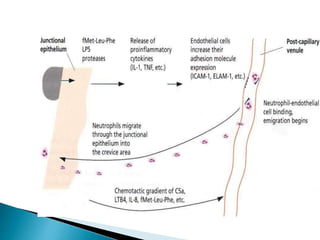
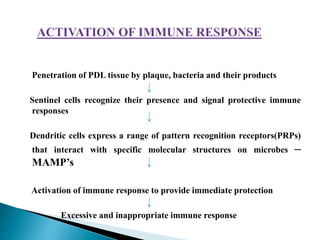
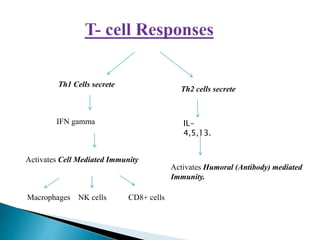
The document discusses the pathogenesis of periodontal disease, detailing the step-by-step processes that lead to tissue changes caused by bacterial challenges and immune responses. It highlights the histopathological stages of gingivitis and periodontitis, emphasizing the role of microbial virulence factors, host immune responses, and their interplay in tissue destruction. Factors such as cytokines, matrix metalloproteinases, and inflammatory mediators significantly influence periodontal inflammation and tissue damage.