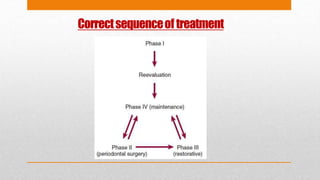
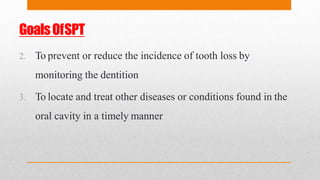
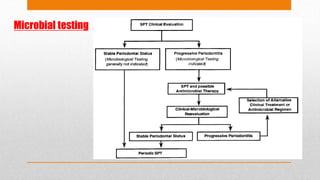
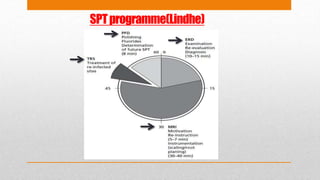
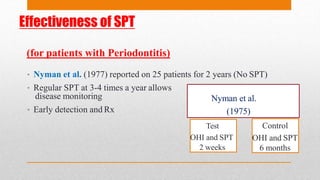
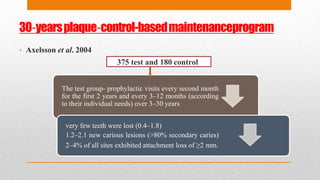
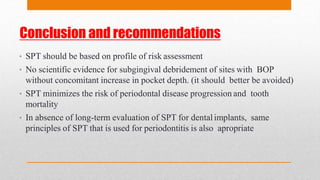
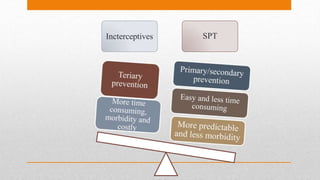
1. Supportive periodontal therapy (SPT) involves procedures performed at regular intervals to help patients maintain oral health after initial periodontal treatment. The goals of SPT include preventing recurrence of periodontal disease and reducing tooth loss through ongoing monitoring.
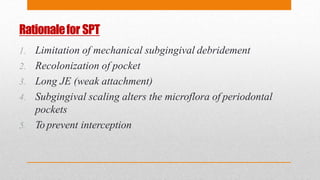
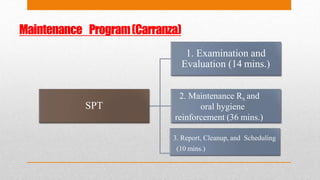
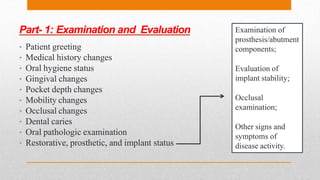
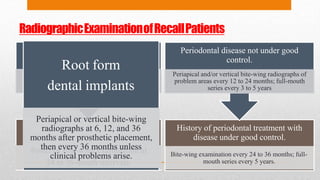
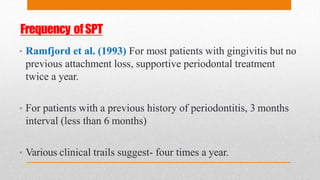
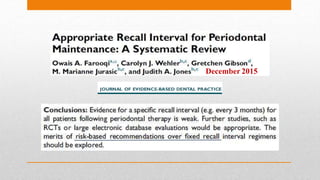
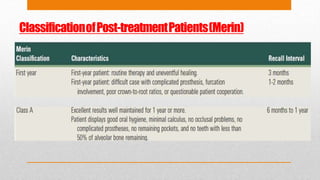
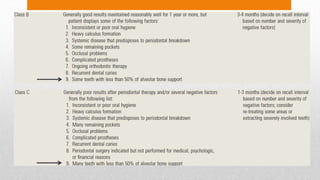
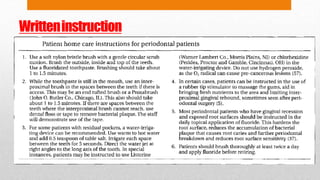
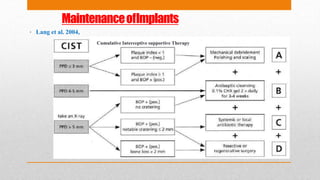
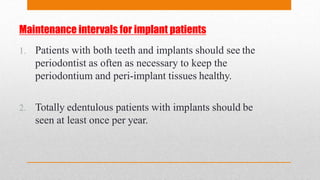
2. SPT consists of examination and evaluation of periodontal health, maintenance treatment such as scaling and oral hygiene reinforcement, and scheduling future visits. Regular SPT at intervals of 3-4 times per year or less has been shown to effectively maintain periodontal health and limit further attachment loss.
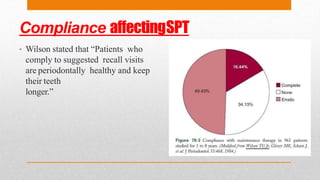
3. Compliance with the SPT regimen is important for achieving positive outcomes. Factors like education, simplified instructions, and positive reinforcement can help improve patient compliance.