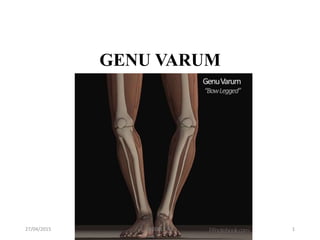
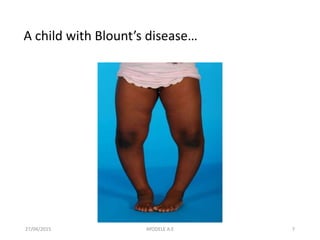
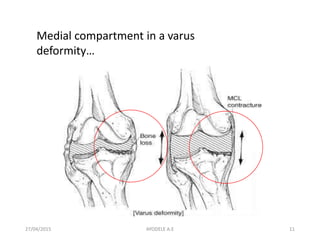
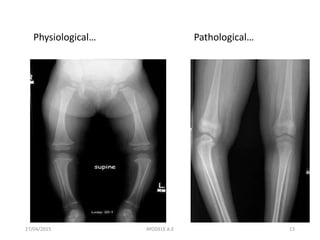
Genu varum, also known as bow legs, is a physical deformity where the legs curve outward from the thighs. It can occur in children due to normal development or due to conditions like Blount's disease or rickets that affect bone growth. In children, genu varum is often monitored and may resolve on its own, while more severe cases or those caused by underlying diseases may require bracing or surgery to correct alignment and prevent long-term issues. Surgical options aim to stop abnormal bone growth or reshape the shinbone to straighten the legs.