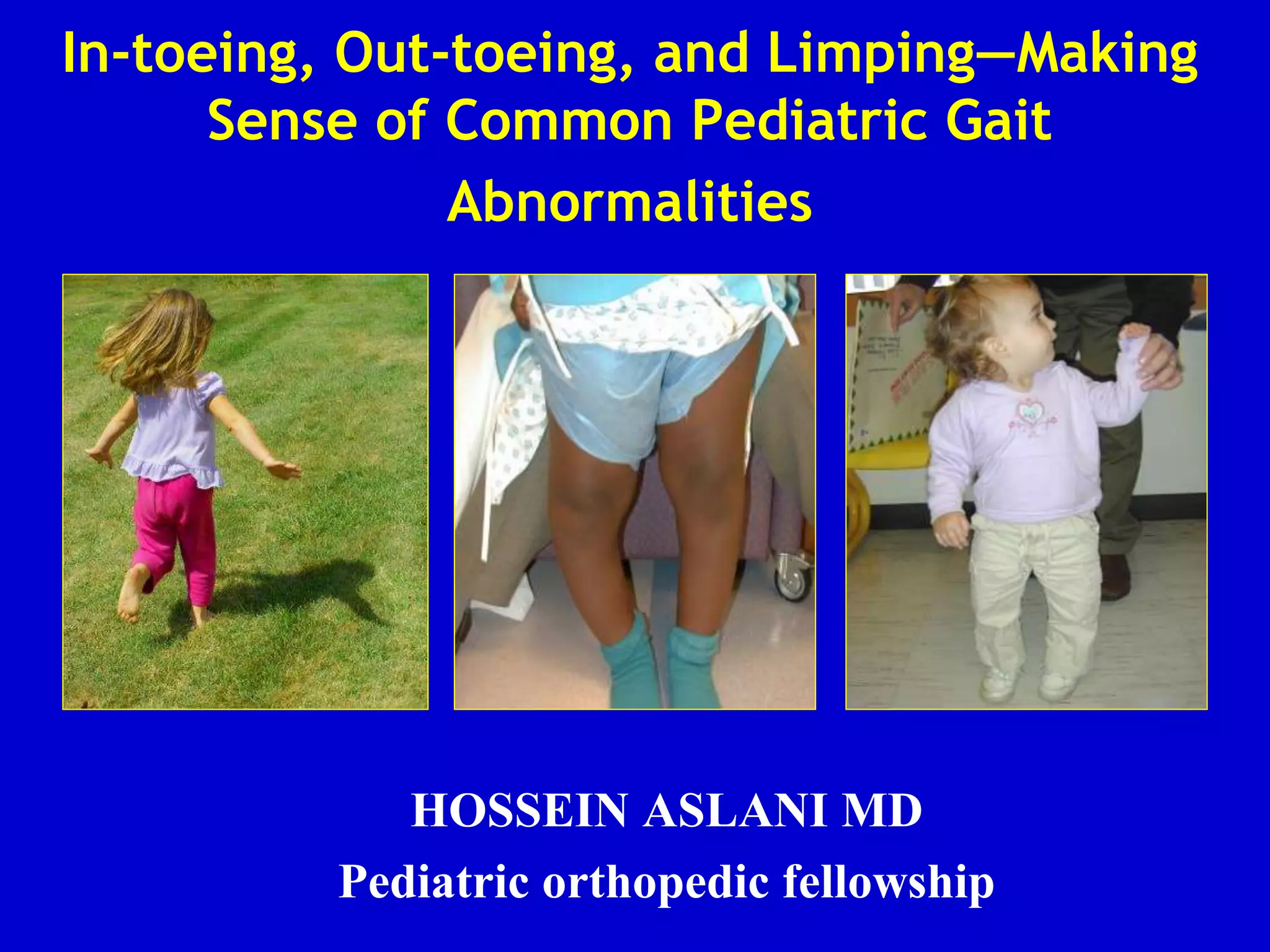
This document discusses common pediatric gait abnormalities including in-toeing, out-toeing, and limping. It reviews the physiologic and pathologic causes of these conditions and provides guidance on physical examination techniques and differential diagnosis. Common causes of in-toeing include femoral anteversion, medial tibial torsion, and metatarsus adductus. Out-toeing is often due to external tibial torsion. Genu valgum (bowlegs) is usually physiologic in young children and resolves on its own, while pathologic causes like rickets require medical treatment. Observation is the typical management for most rotational and angular deformities in children as they often correct spontaneously with growth.






































![Physiologic Genu Varum: Assessment
• Parents will often note bow leg
deformity, usually recognized
when child starts to walk (12-18
months)
• Commonly bilateral and
symmetric bowing
• Seldom causes functional
disability [X-rays unnecessary
until at least 18 months of age]
• Physiologic bowing usually
spontaneously resolves by the age
of two years](https://image.slidesharecdn.com/gaitabnormalitiesinchildren-221215093450-3e9183e5/85/gait-abnormalities-in-children-ppt-40-320.jpg)


























