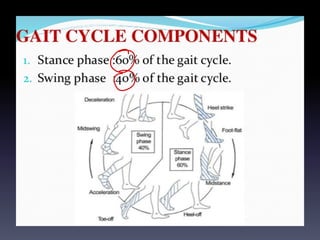
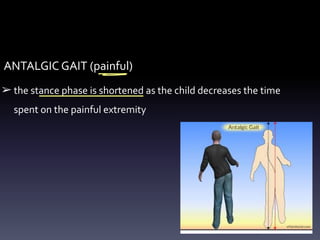
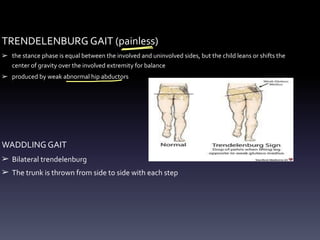
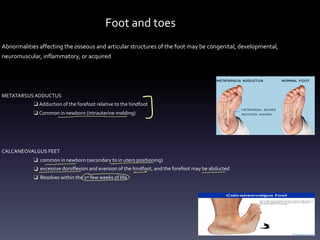
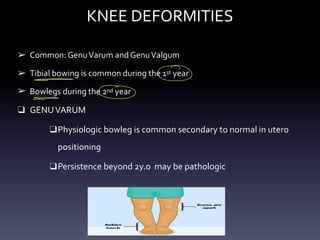
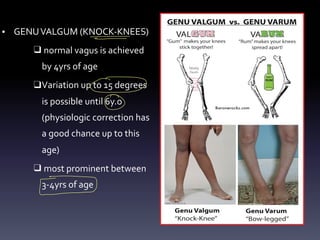
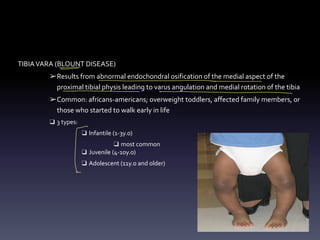
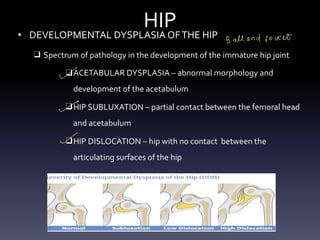
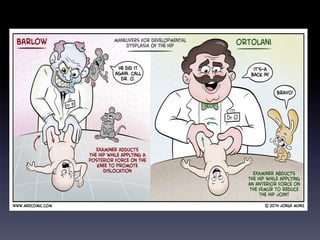
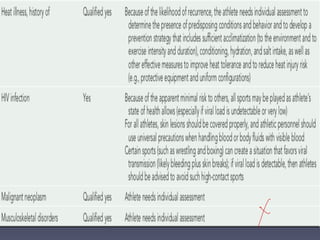
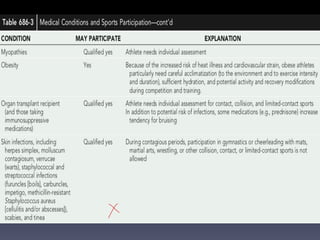
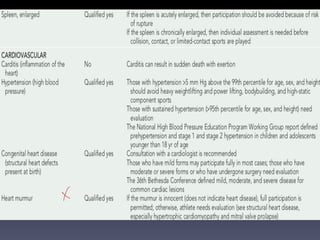
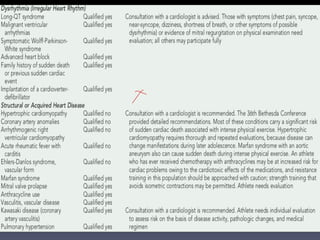
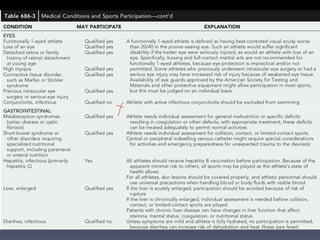
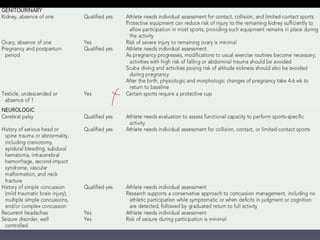
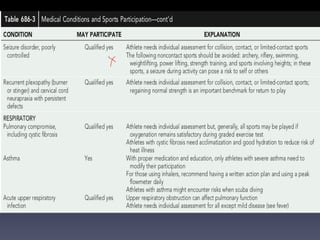
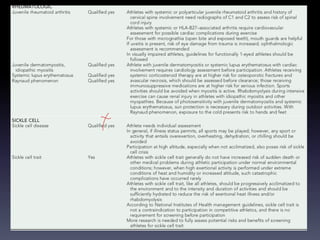
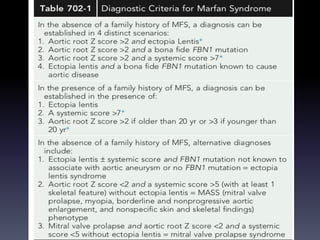
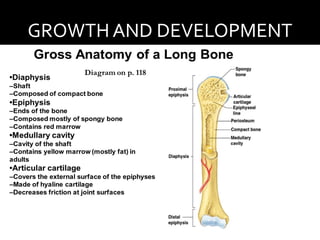
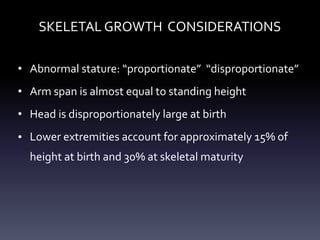
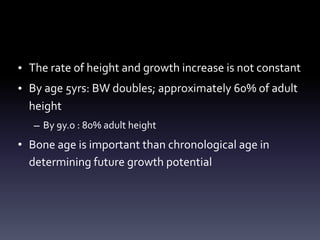
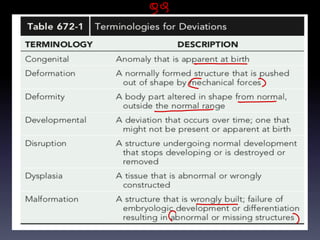
The document discusses pediatric orthopaedic bone and joint disorders, highlighting skeletal growth, evaluation methods, and common conditions affecting children. It covers various disorders such as genu varum, developmental dysplasia of the hip, and scoliosis, including their definitions, assessments, and treatment options. Key topics also include gait analysis and diagnostic imaging techniques essential for evaluating musculoskeletal disorders in pediatrics.
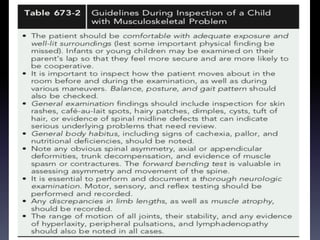
![PALPATION
Assessment of local
temperature and
tenderness; swelling or
mass, spasticity or
contracture, bone or joint
deformity, evaluation of
anatomic axis of limb and
limb lengths
spasticity]
Contracture
↳ Congenital](https://image.slidesharecdn.com/36-240427002036-7bcf1aa7/85/36-BONES-AND-JOINTS-DISORDER-pediatrics-12-320.jpg)