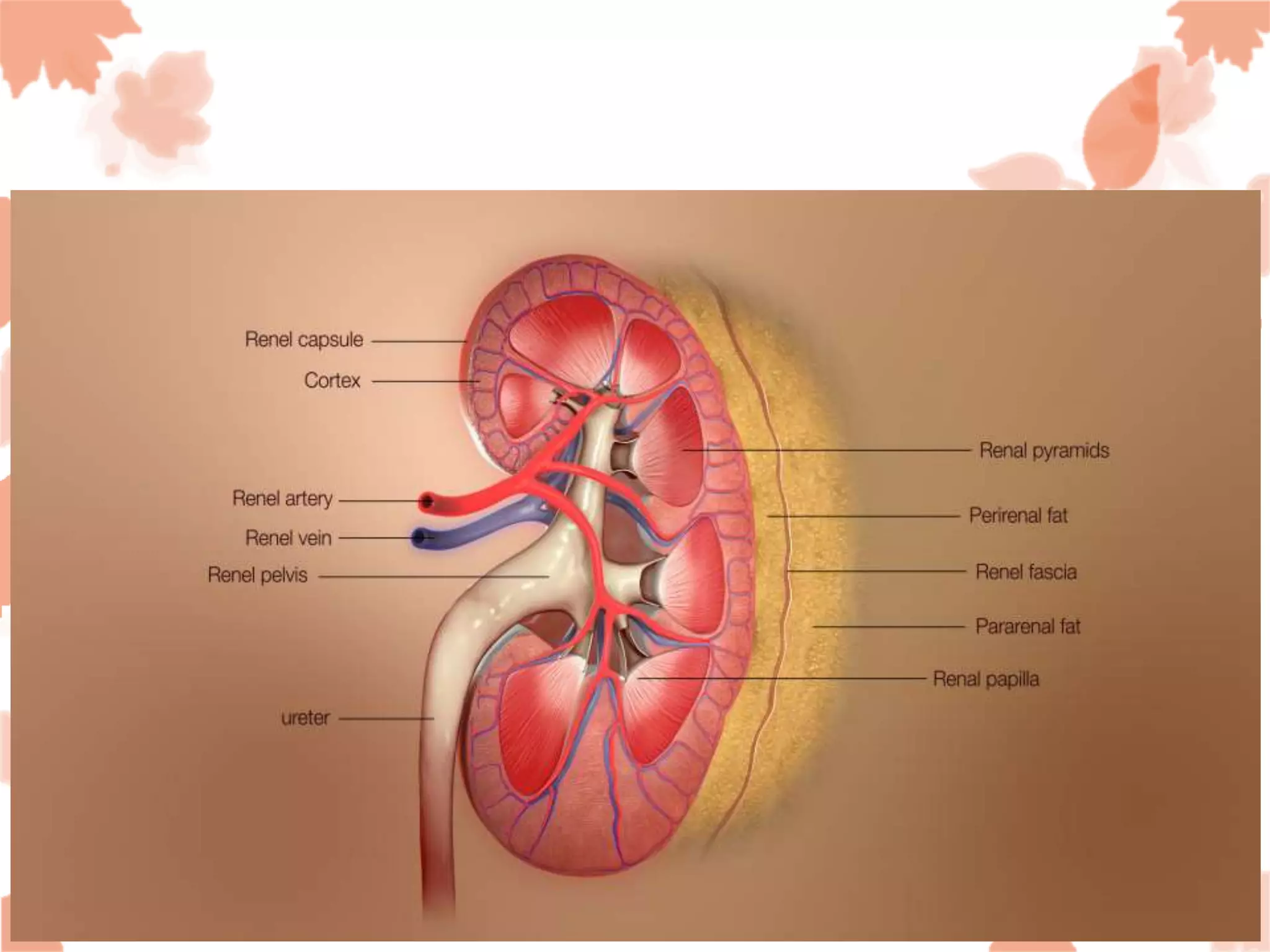
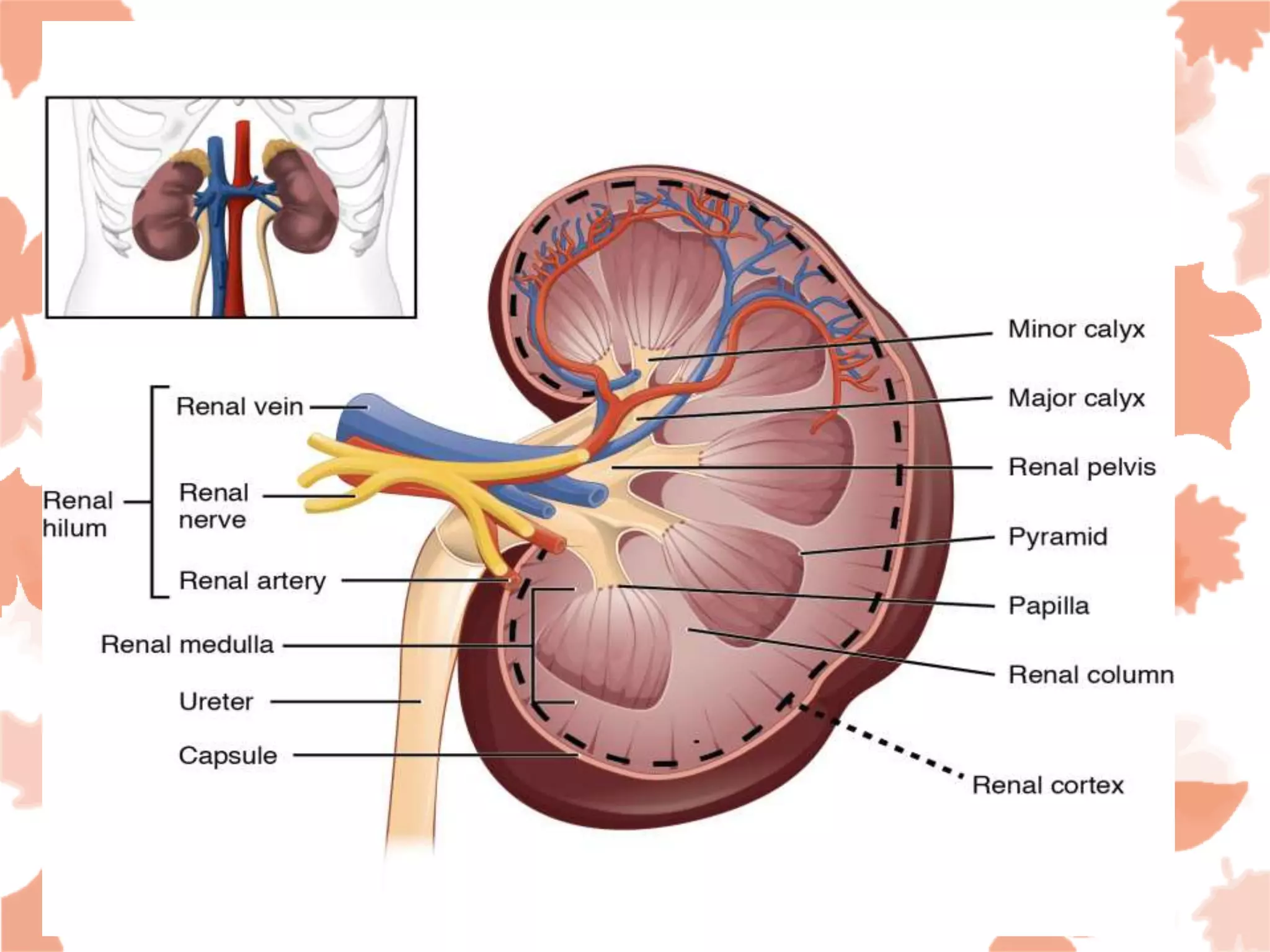
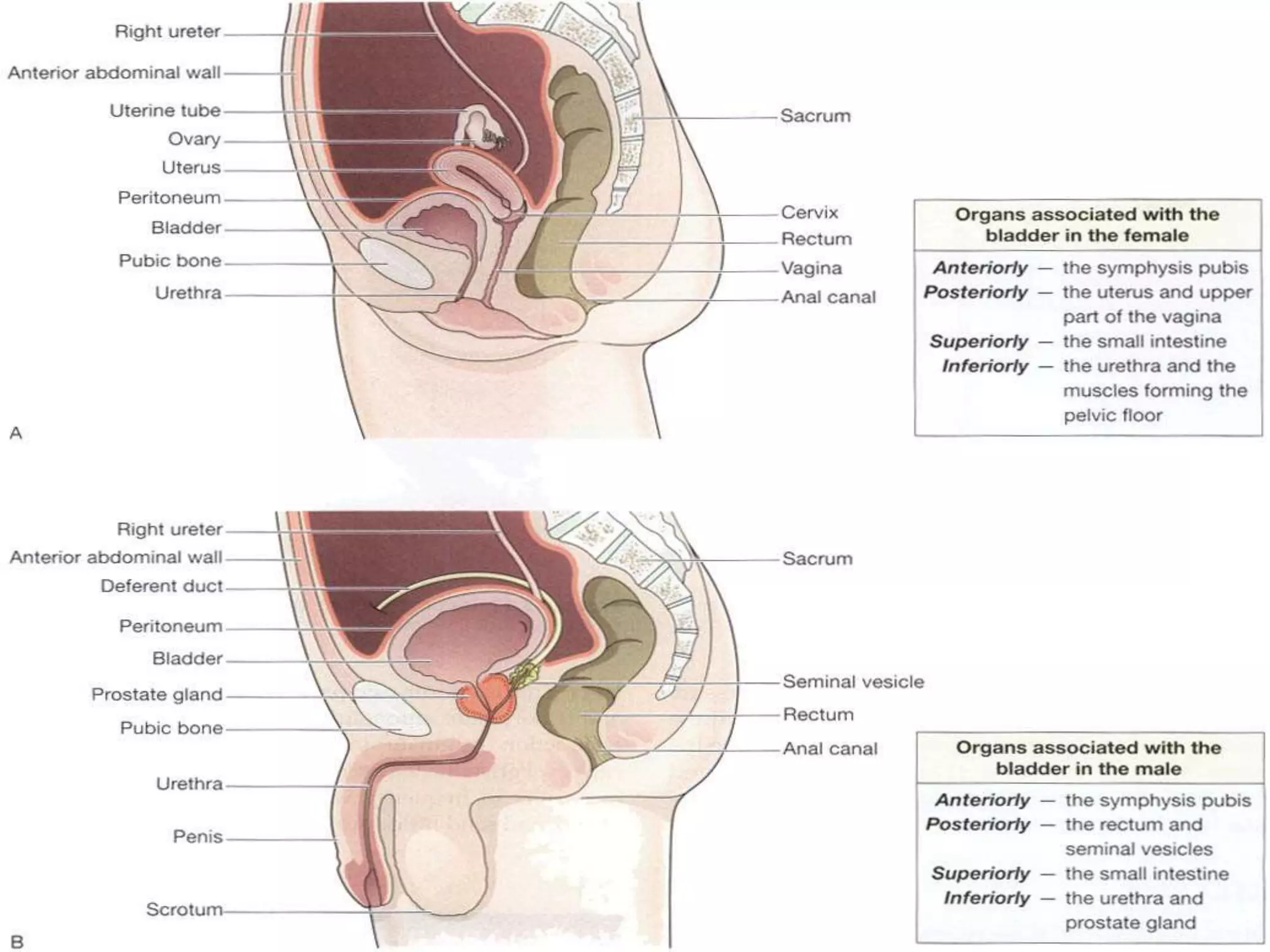
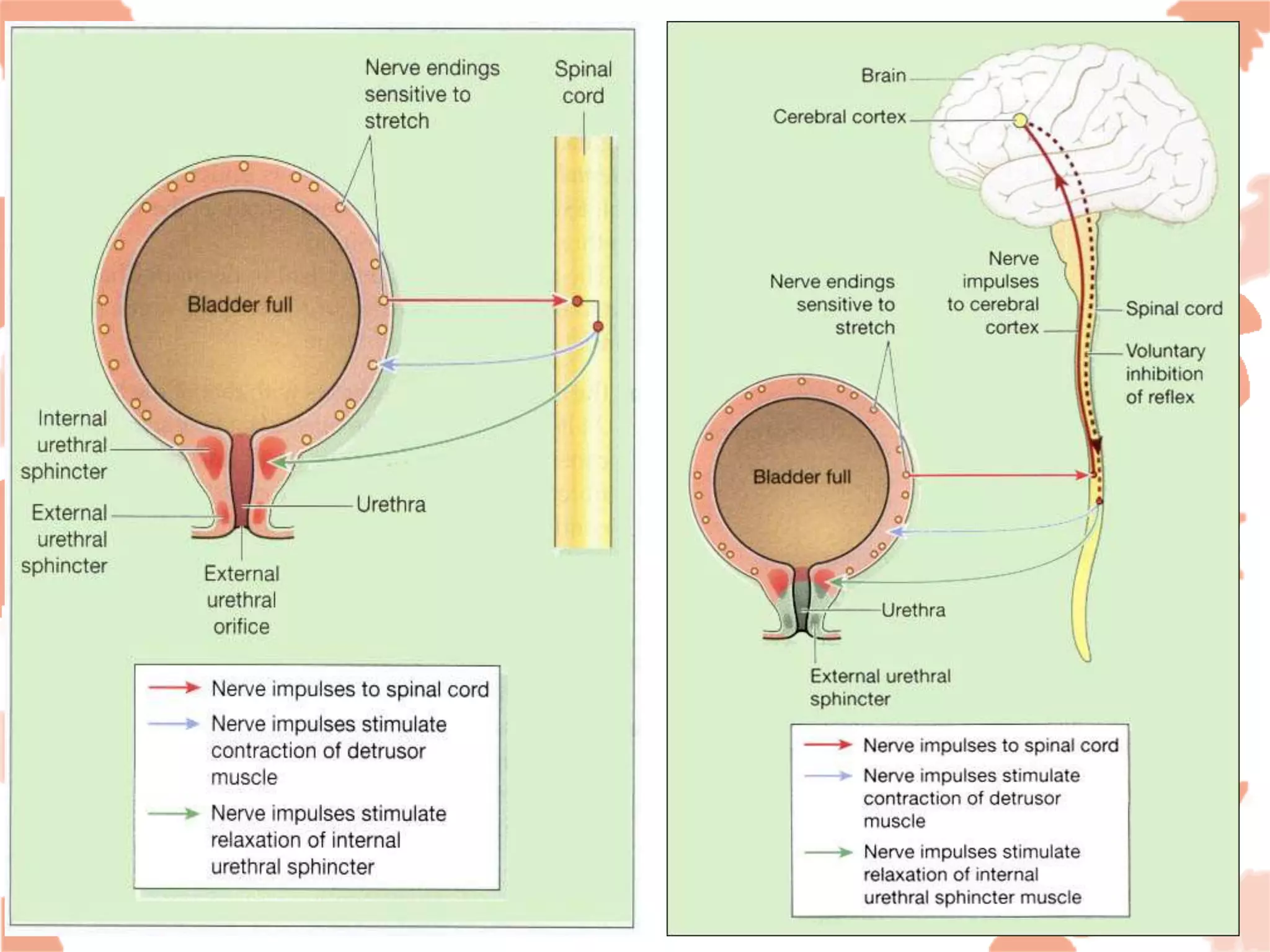
The urinary system consists of the kidneys, ureters, bladder, and urethra, playing a crucial role in excretion and maintaining homeostasis of water and electrolytes. The kidneys produce urine that contains metabolic waste and various substances, while the bladder serves as a reservoir for urine until micturition occurs. The document also discusses kidney diseases, urinary tract infections, and incontinence, highlighting their causes and effects.