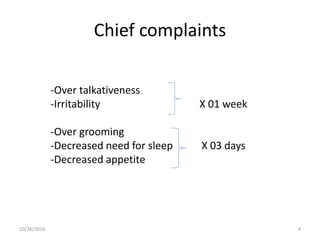
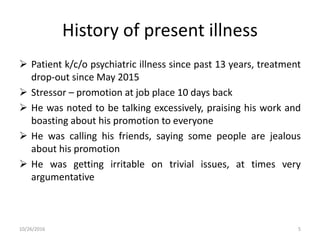
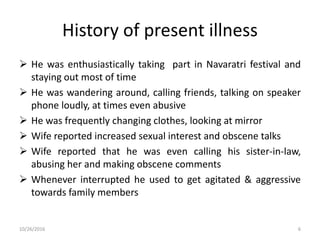
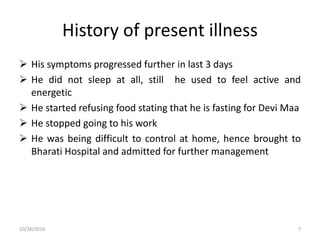
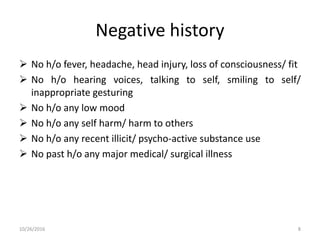
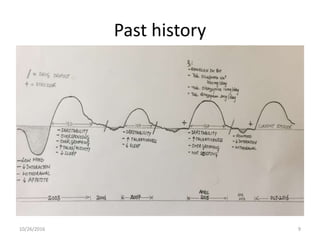
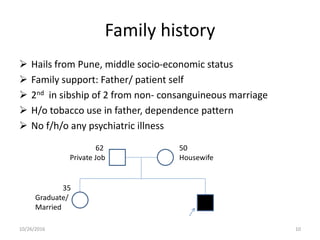
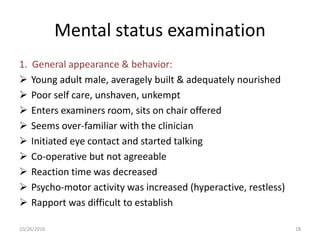
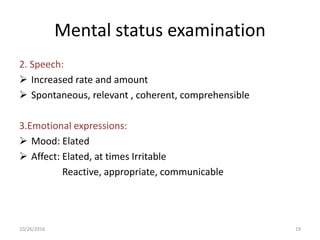
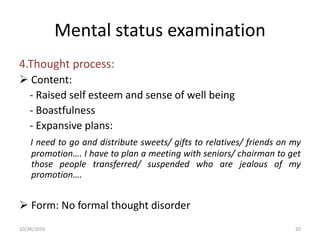
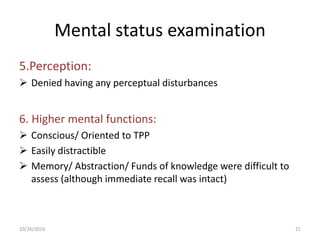
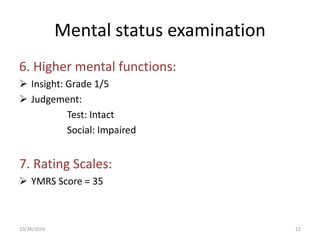
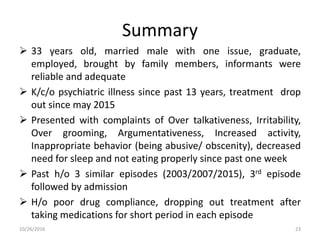
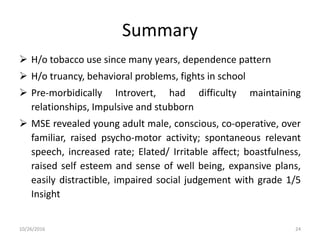
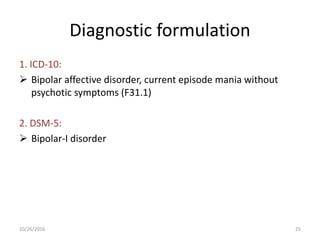
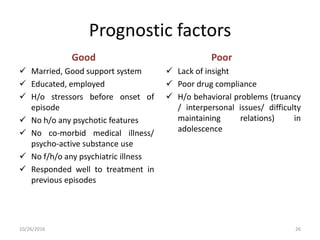
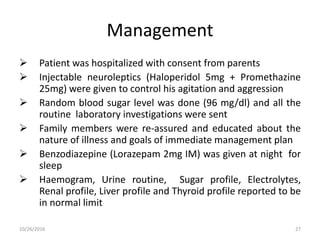
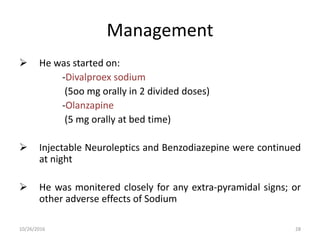
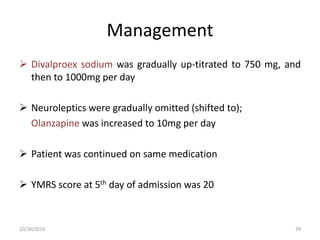
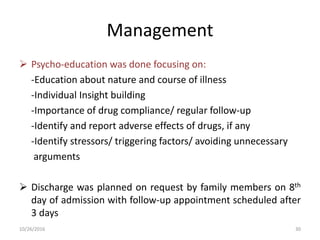
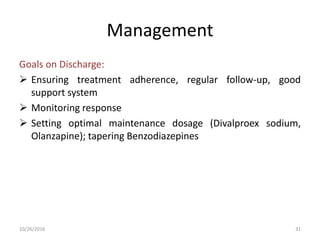
A 33-year-old male with an extensive history of psychiatric illness presented with symptoms of over talkativeness, irritability, and inappropriate behavior following a job promotion, leading to hospitalization. Diagnosed with bipolar affective disorder, he received a combination of medications including neuroleptics and mood stabilizers, alongside psychoeducation for his family. The treatment plan emphasized regular follow-up and monitoring to ensure medication adherence and proper management of his condition.