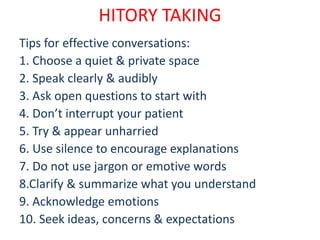
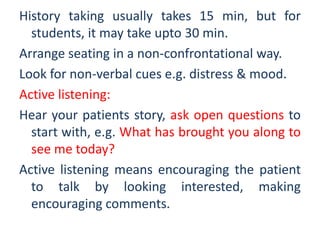
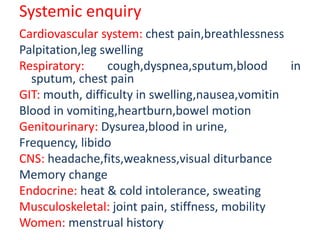
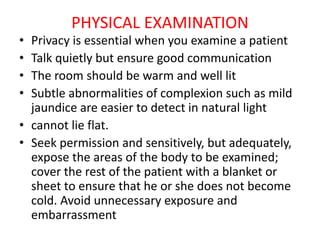
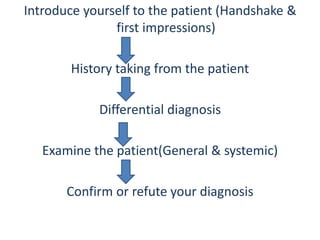
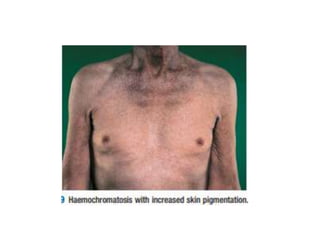
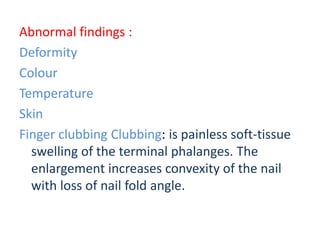
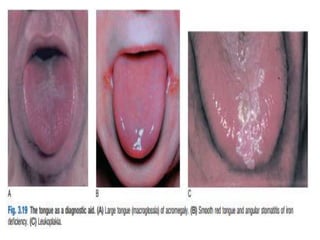
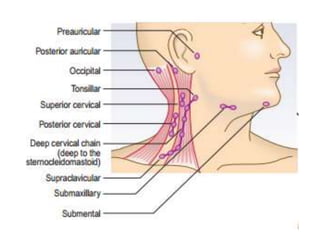
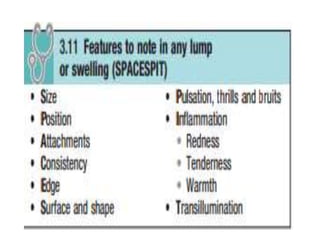
This document provides guidance on performing a patient history and physical examination. It outlines important tips for effective history taking, including choosing a quiet space, asking open-ended questions, active listening, and clarifying information. The history should obtain demographic data, chief complaint, history of present illness, past medical history, drug history, family history, and social history. The physical exam involves inspection, palpation, percussion, and auscultation of general appearance and different body systems. Proper patient positioning, draping, and communication are important. Notable findings on exam may include clubbing, cyanosis, rashes, or enlarged lymph nodes.