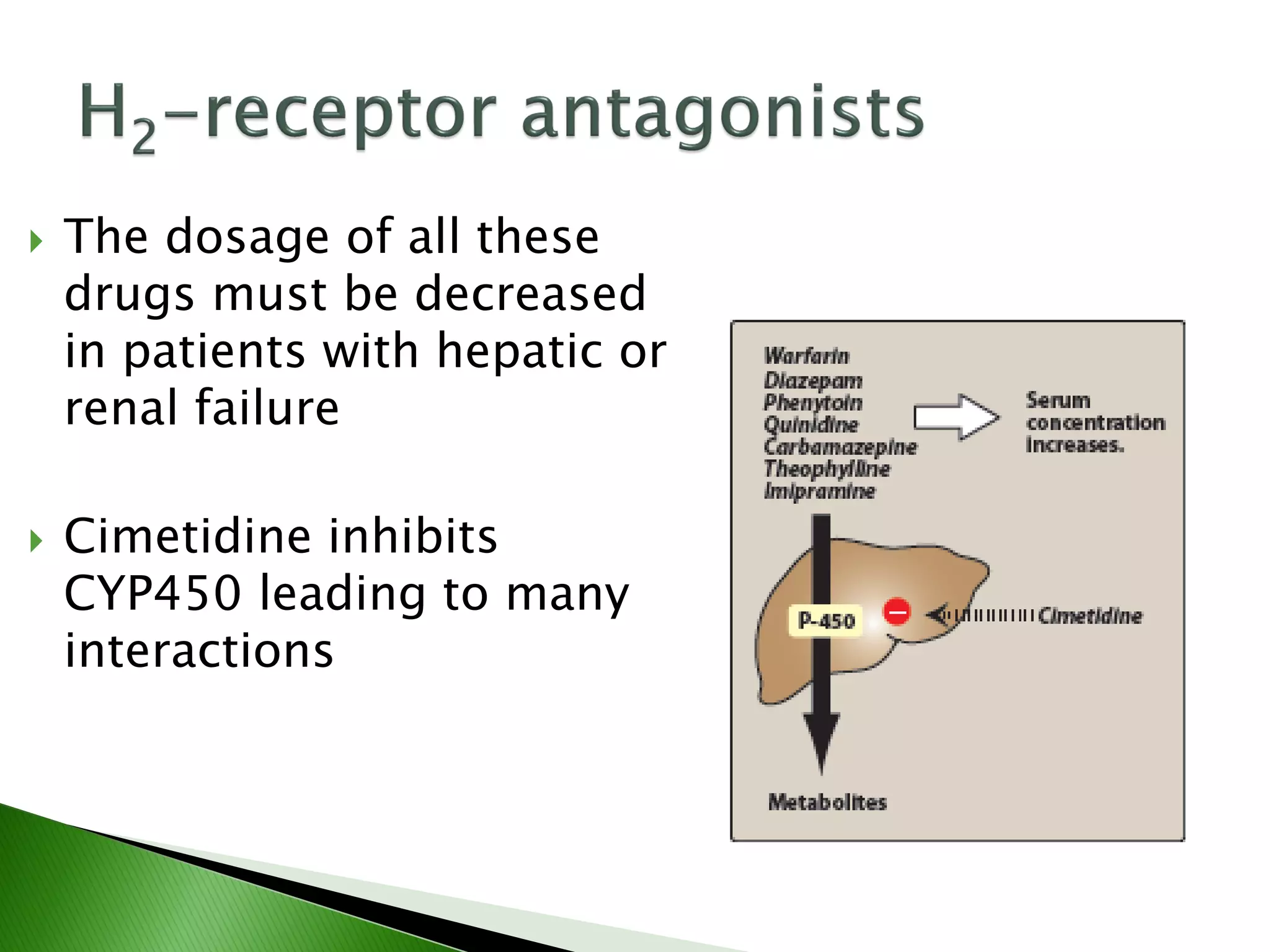
The document discusses drugs used to treat peptic ulcers, gastroesophageal reflux disease, diarrhea, and constipation. It describes the causes of peptic ulcers including H. pylori infection and NSAID use. Treatment involves eradicating H. pylori, reducing gastric acid with H2 blockers or proton pump inhibitors, and protecting the gastric mucosa. Various classes of drugs are covered that act on these mechanisms including antimicrobials, H2 blockers, proton pump inhibitors, prostaglandins, and antacids.