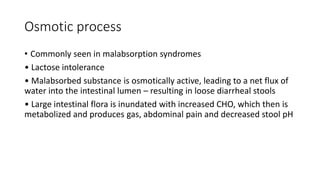
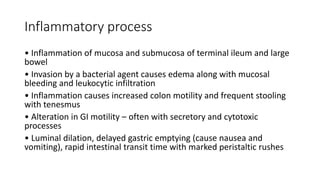
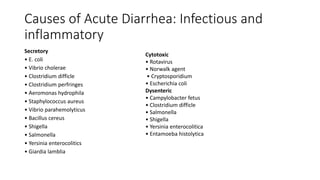
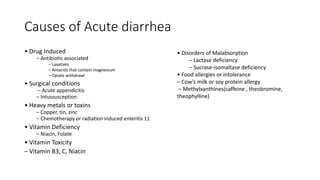
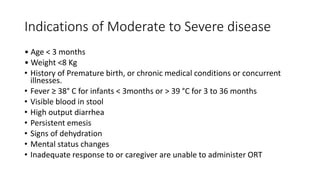
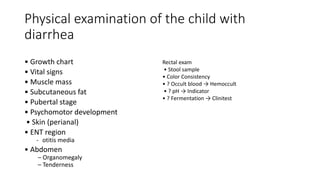
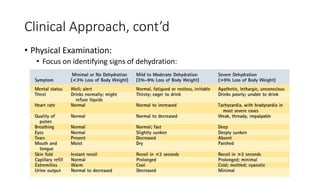
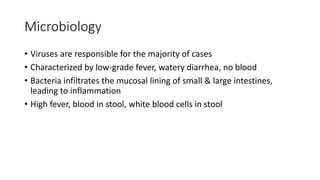
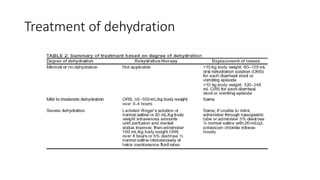
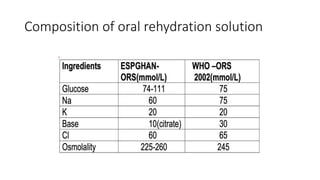
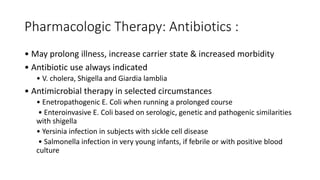
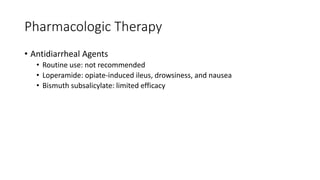
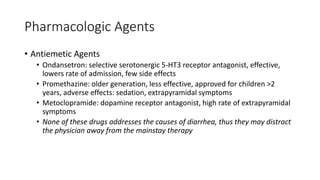
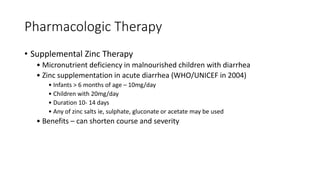
The document provides a detailed overview of acute gastroenteritis in children, focusing on diagnosis and management according to the latest guidelines. It emphasizes the importance of early rehydration, the outdated nature of 'bowel rest', and discourages the use of antidiarrheal agents. It also highlights effective treatment options such as oral rehydration solutions, zinc supplementation, and probiotics, while stressing prevention through education and sanitation.