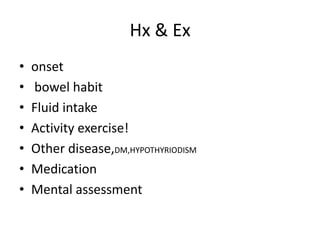
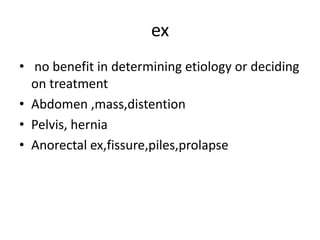
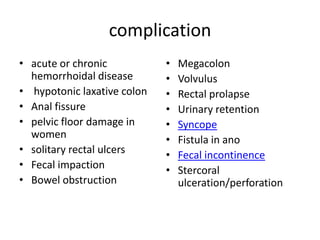
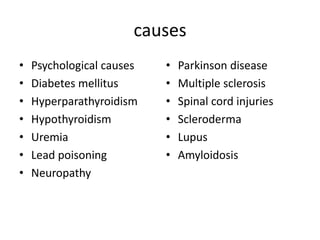
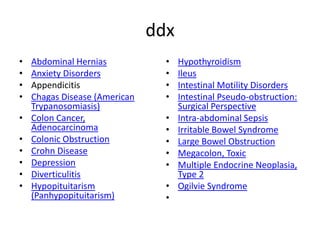
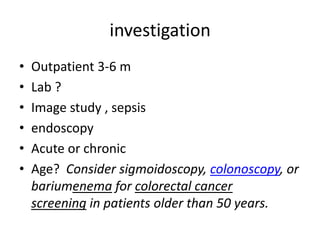
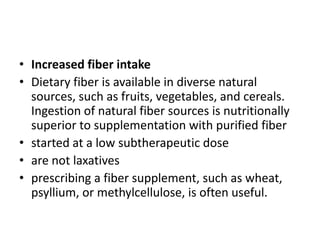
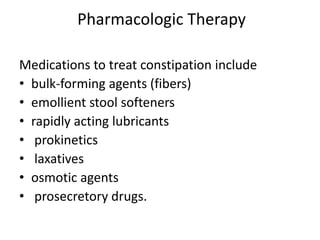
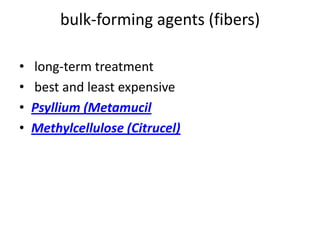
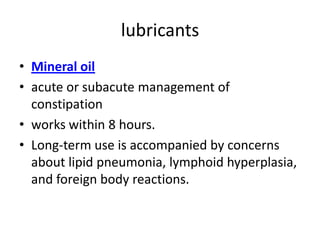
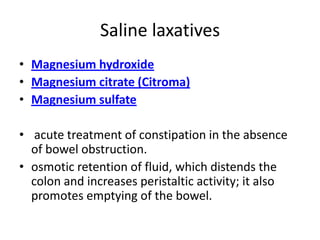
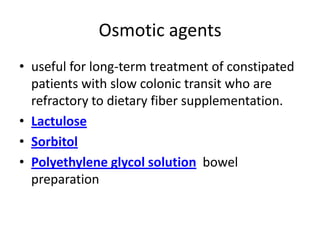
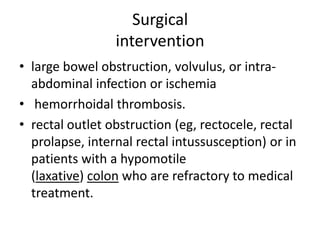
This document defines constipation and outlines its causes, symptoms, diagnosis, and treatment options. Constipation is a common condition affecting approximately 2% of the US population. It is defined as having less than 3 bowel movements per week or experiencing straining with defecation. Causes can include low fiber diet, lack of exercise, certain medications, and underlying medical conditions. Treatment focuses on increasing fiber and fluid intake, exercise, stool softeners, laxatives, and if needed, surgery to address complications. Long term monitoring may involve screening for underlying causes and ensuring dietary and medication management is effective.
![• Rectal bleeding
• Abdominal pain (suggestive of
possible irritable bowel syndrome [IBS] with
constipation [IBS-C])
• Inability to pass flatus
• Vomiting
• Unexplained weight loss](https://image.slidesharecdn.com/constipation-140309225027-phpapp01/85/Constipation-9-320.jpg)