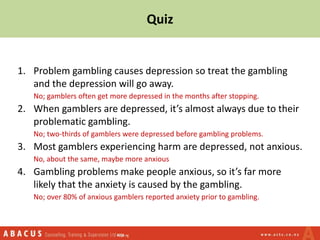
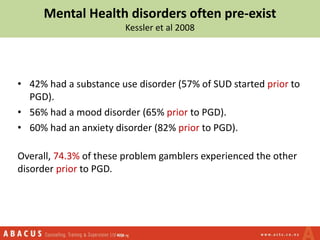
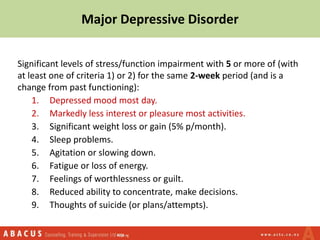
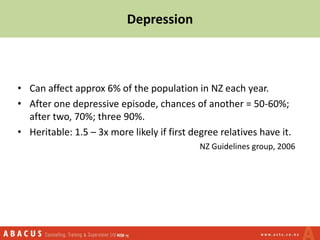
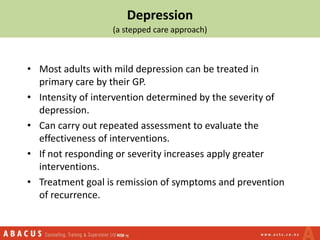
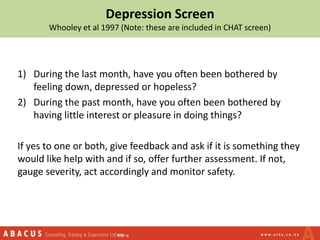
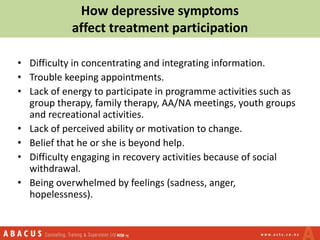
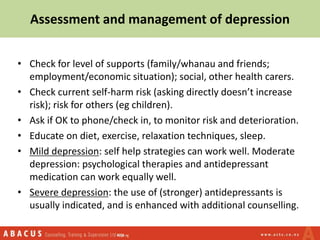
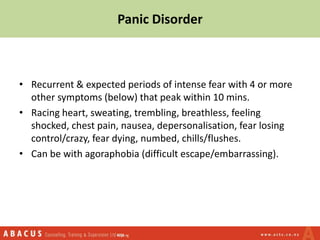
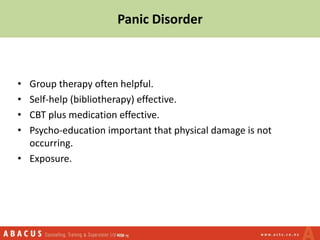
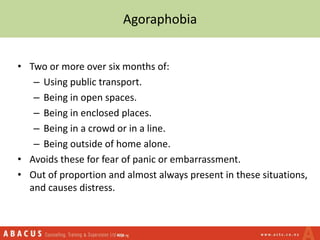
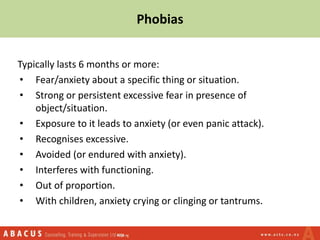
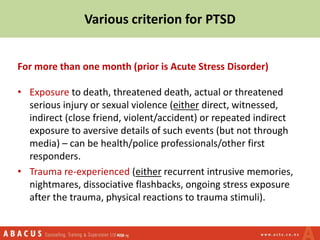
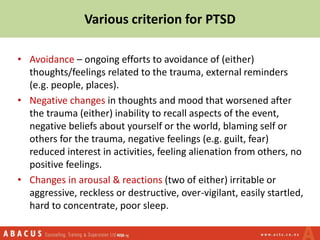
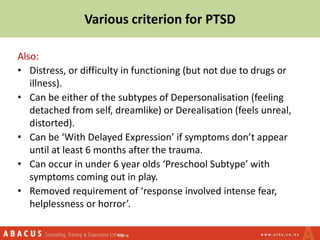
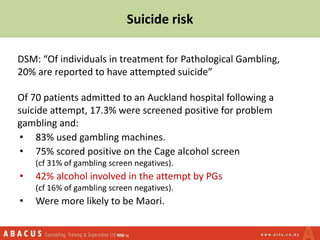
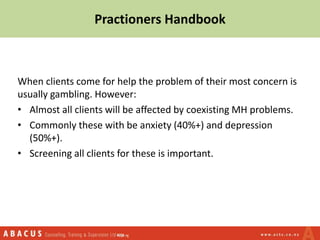
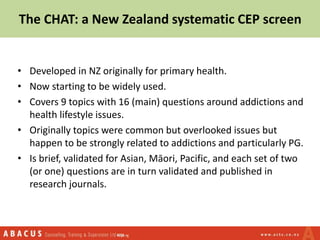
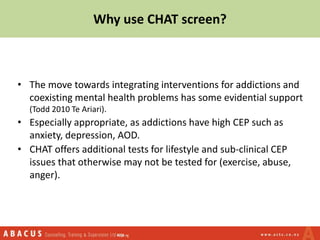
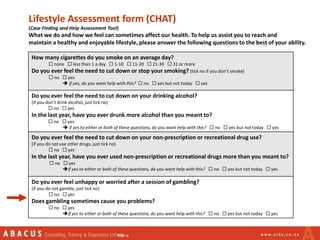
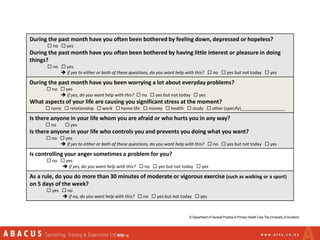
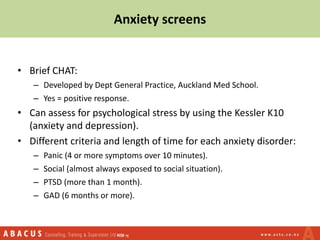
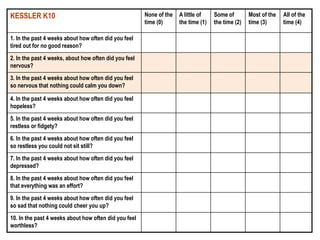
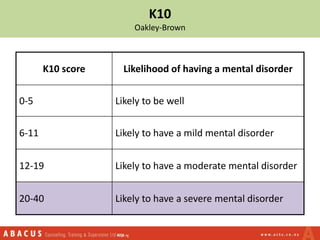
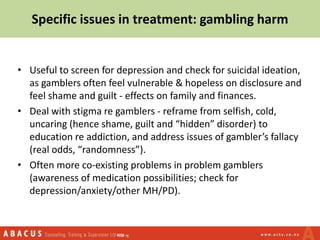
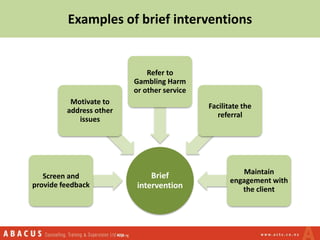
This document discusses anxiety, depression, and their relationship to problem gambling. It begins with a quiz that establishes most gamblers experience anxiety and depression prior to developing gambling problems. It then cites a study that found 74.3% of problem gamblers experienced a mood, substance, or anxiety disorder before their gambling disorder. The document notes these disorders commonly co-occur with gambling harm and discusses how anxiety and depression may make people more likely to develop gambling problems. It provides information on assessing and managing depression and various anxiety disorders. Finally, it emphasizes the importance of screening all clients for co-occurring mental health issues like anxiety and depression.