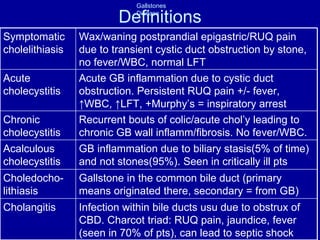
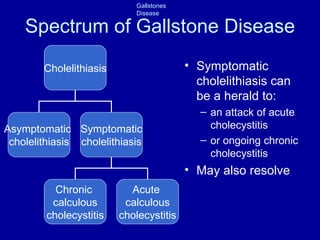
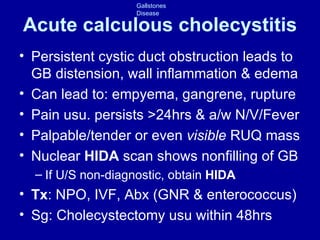
1. Gallstone disease ranges from asymptomatic cholelithiasis to complications like acute cholecystitis, cholangitis, or pancreatitis. The pathophysiology involves cholesterol supersaturation in bile leading to stone formation over three stages.
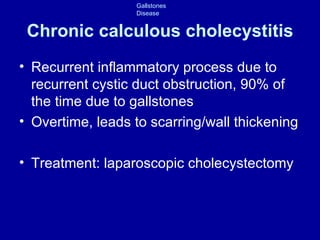
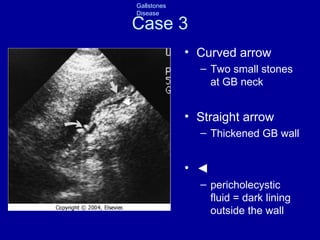
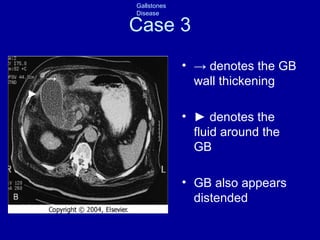
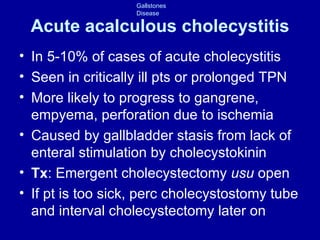
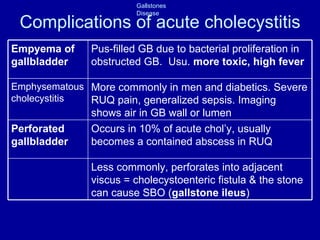
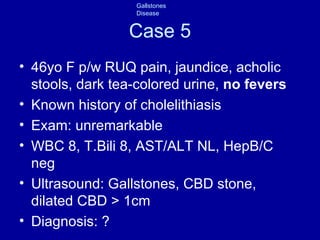
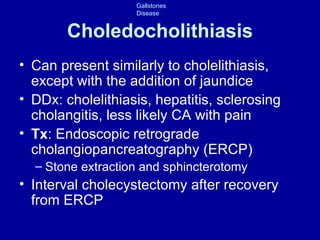
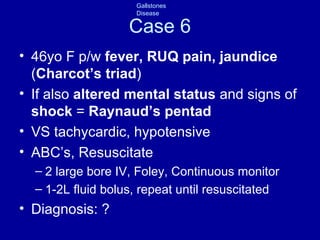
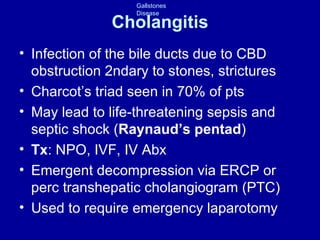
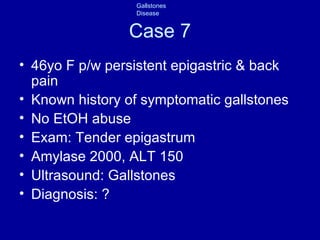
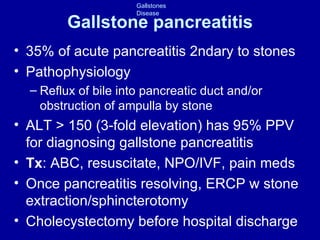
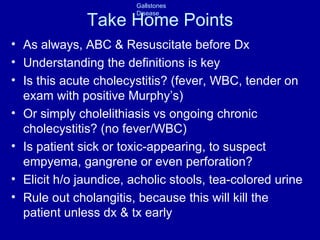
2. Seven cases demonstrate the clinical presentations of symptomatic cholelithiasis, chronic cholecystitis, acute cholecystitis, acalculous cholecystitis, choledocholithiasis, cholangitis, and gallstone pancreatitis. Diagnosis involves the history, exam, labs, and imaging findings specific to each condition.
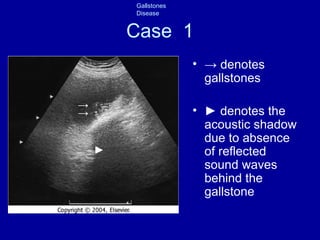
3. Treatment depends on the condition but may include antibiotics, endoscopic retrograde cholangiop