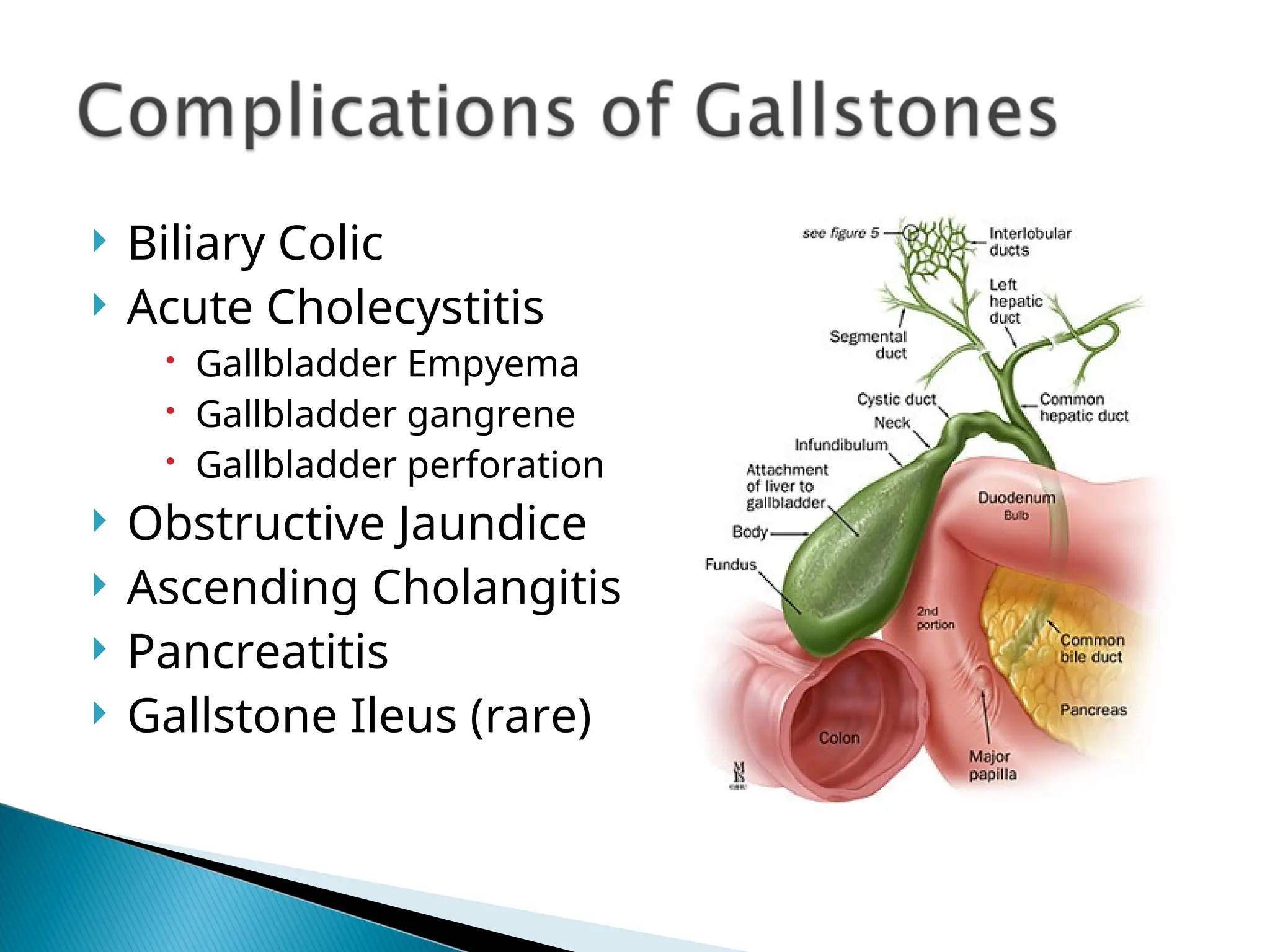
The document provides an overview of gallstone types, their epidemiology, composition of bile, complications, and diagnostic/testing methods. It discusses the clinical presentations of various gallstone-related conditions, treatment options, and the timing for surgical interventions like cholecystectomy. The focus is on understanding the pathophysiology, management of complications such as acute cholecystitis and pancreatitis, and the necessity for prompt treatment to avoid life-threatening outcomes.