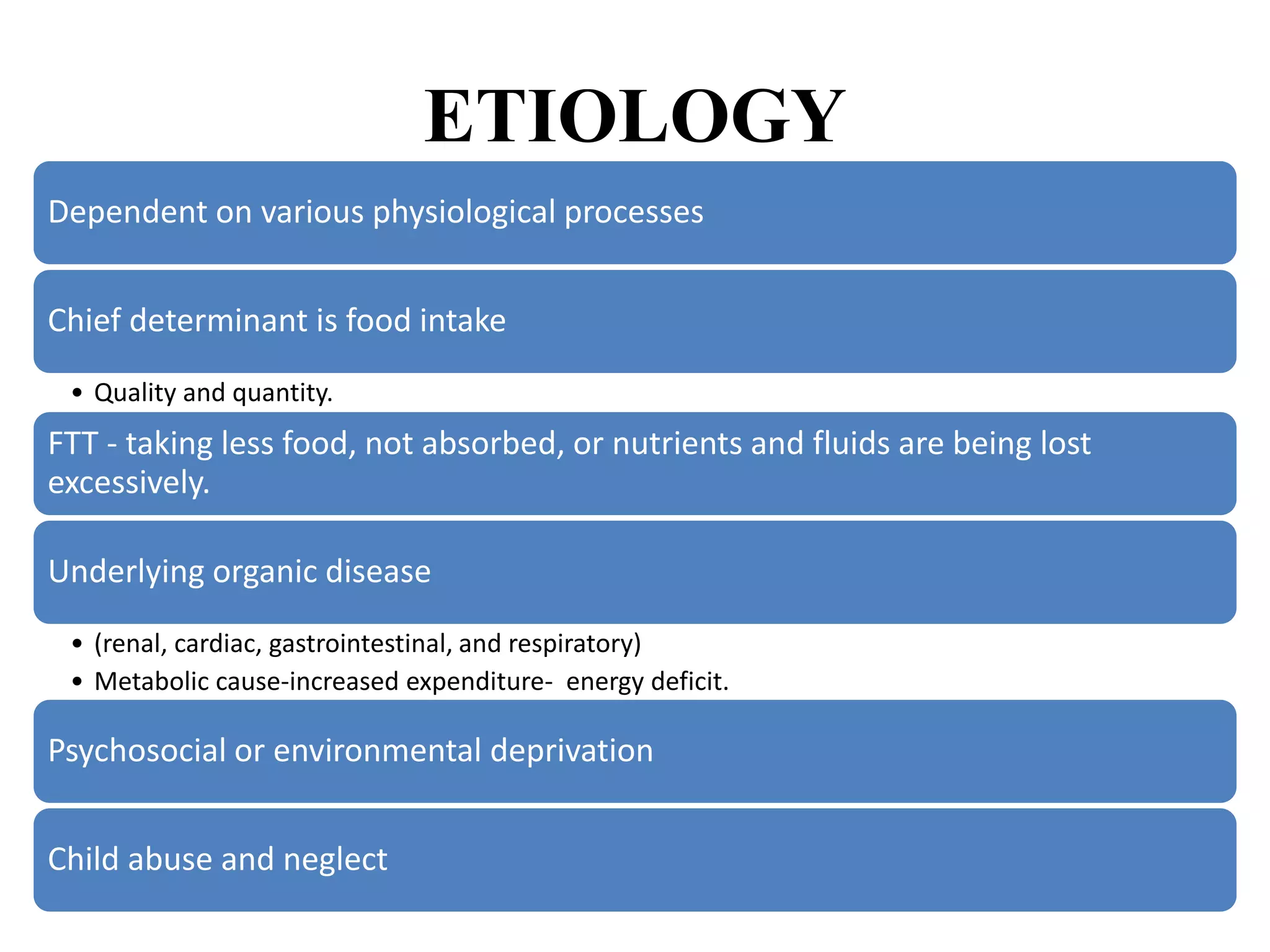
This document discusses failure to thrive and short stature in children. It defines failure to thrive as inadequate calorie intake to support a child's growth and metabolic demands, resulting in growth failure. Causes of failure to thrive include inadequate nutrition from medical issues, psychosocial factors, or increased calorie expenditure from illness or disease. The assessment and management of failure to thrive involves detailed history, examinations to identify underlying causes, nutritional rehabilitation, parental counselling, and medical treatment. Short stature is defined as height below the 3rd percentile or 2 standard deviations below the mean for age and sex. The document discusses normal growth velocity and the determinants of child growth.






























![Calculation of midparental height (MPH)
• MPH (boy) = (Father's height + Mother's height + 13)/2, or
– [(Father's height + Mother's height)/2] +6.5
• MPH (girls) = (Father's height + Mother's height - 13)/2, or
– [(Father's height + Mother's height)/2] - 6.5](https://image.slidesharecdn.com/fttshortstature-230320063223-828fd601/75/FTT-Short-Stature-pptx-35-2048.jpg)