The document discusses identification, pathophysiology, screening, and treatment of severe acute malnutrition (SAM) in infants and children. Key points include:
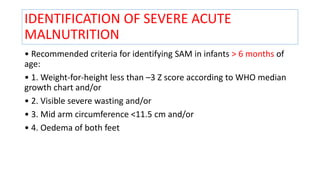
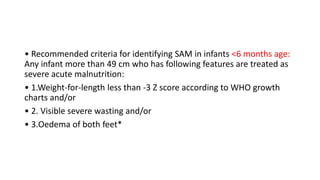
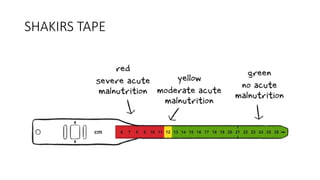
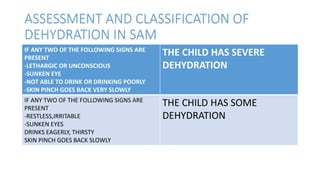
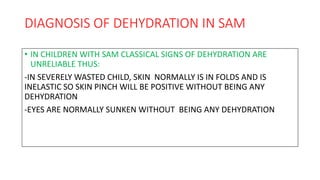
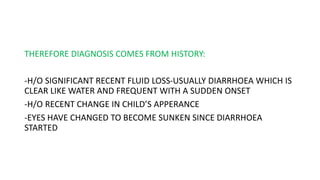
- Recommended criteria for identifying SAM include weight-for-height, mid-upper arm circumference, edema, and visible wasting.
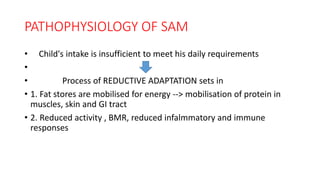
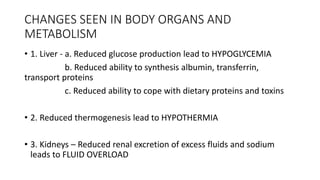
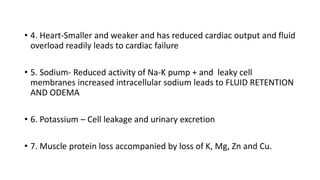
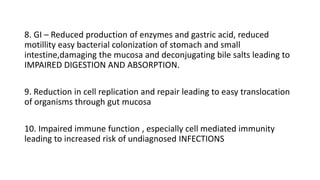
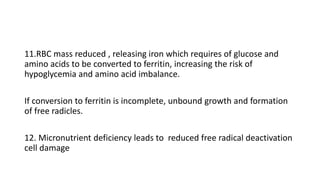
- SAM results from insufficient intake to meet needs, leading to fat and muscle breakdown and impaired organ function.
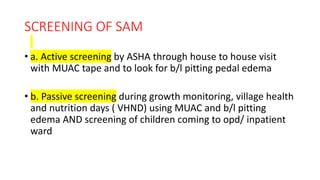
- Screening is done through home visits or at health centers using MUAC tapes and checking for edema.
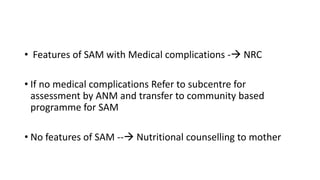
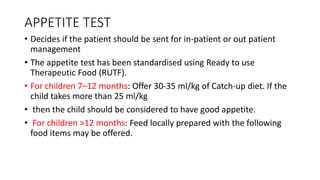
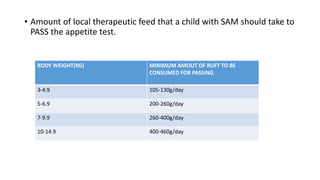
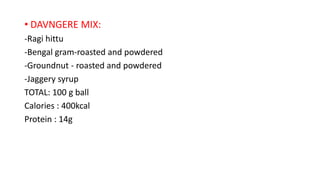
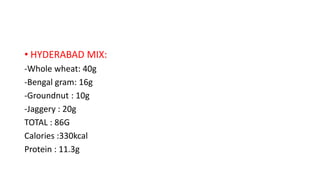
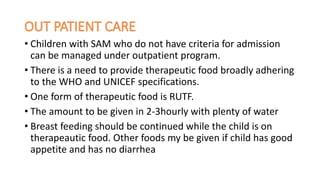
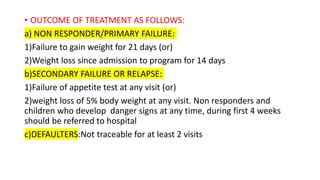
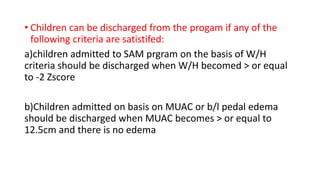
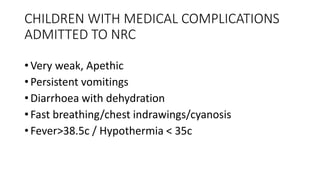
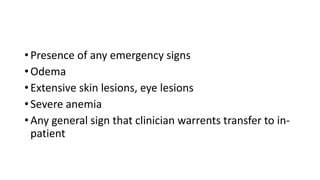
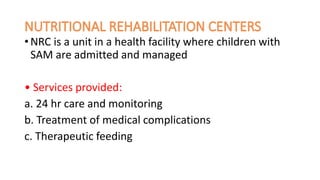
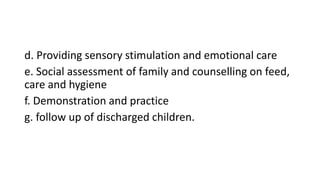
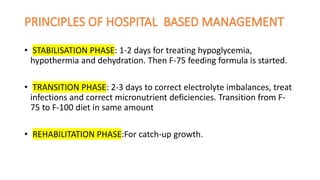
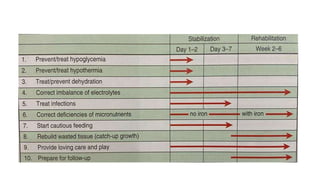
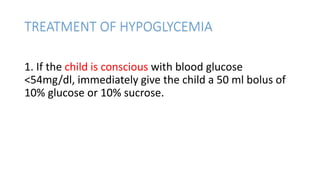
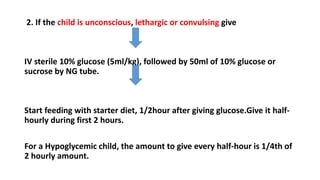
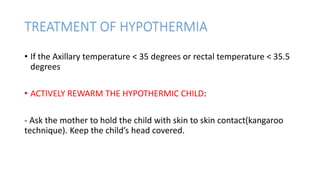
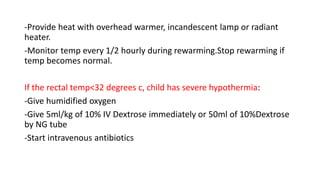
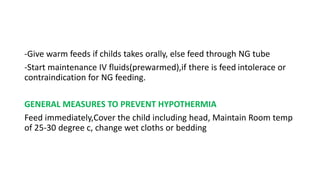
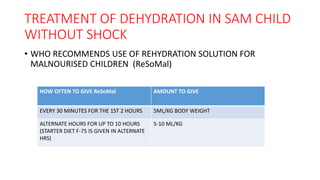
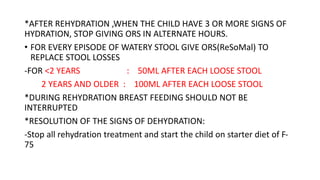
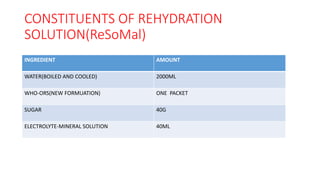
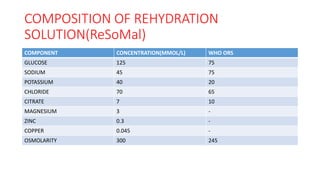
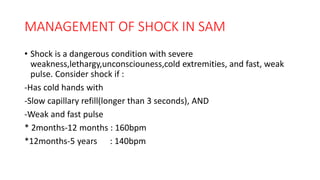
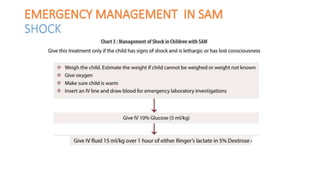
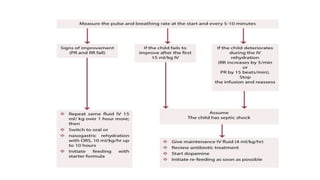
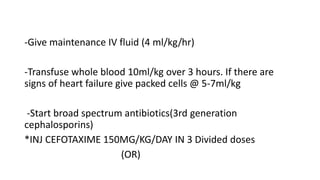
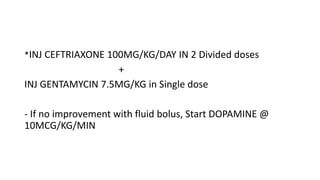
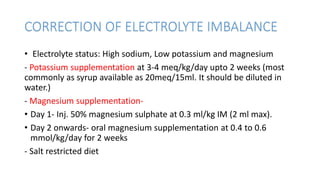
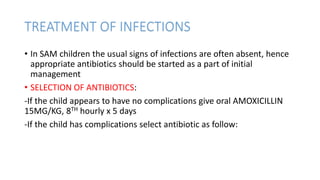
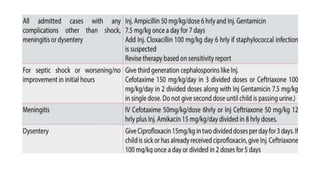
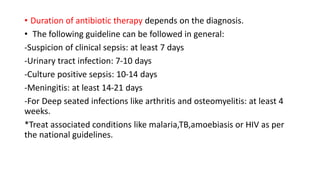
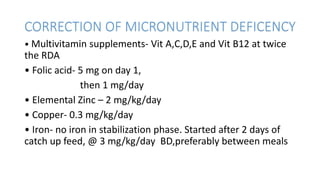
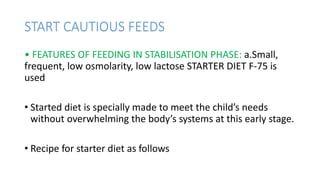
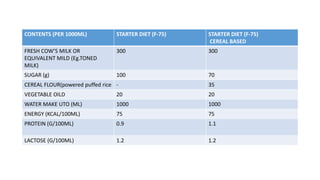
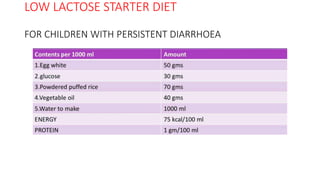
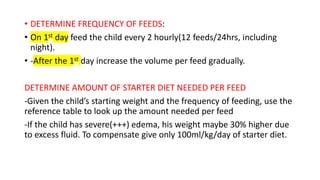
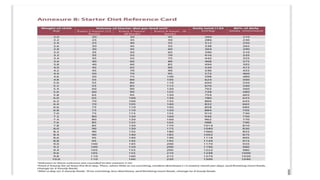
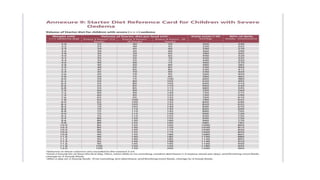
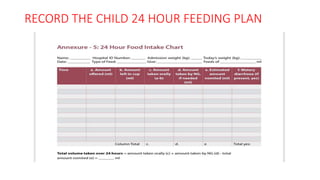
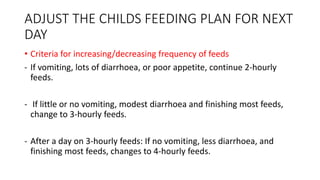
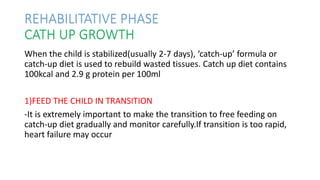
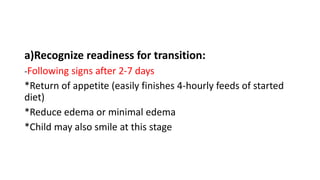
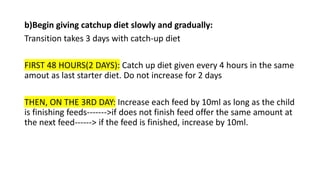
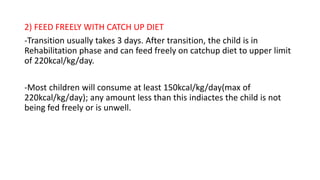
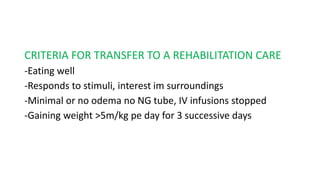
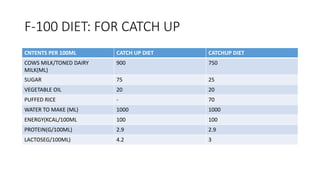
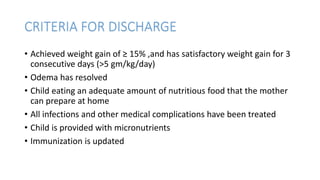
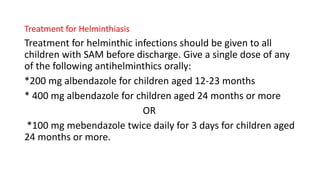
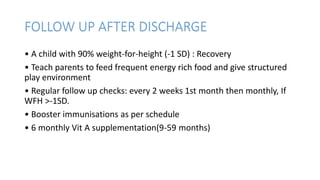
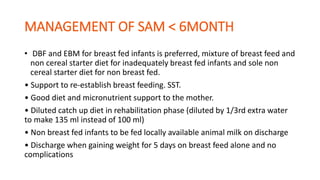
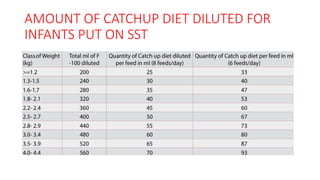
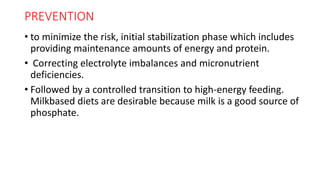
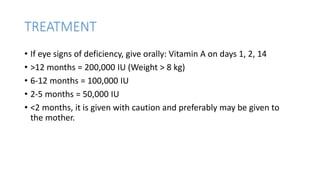
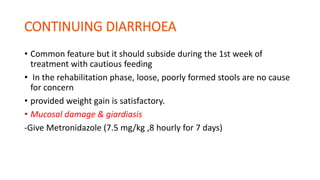
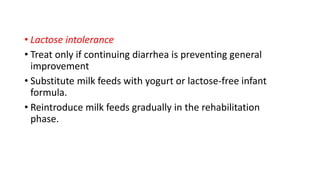
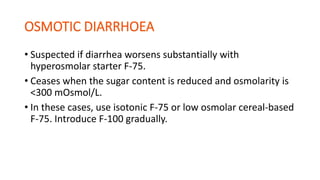
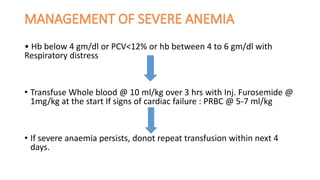
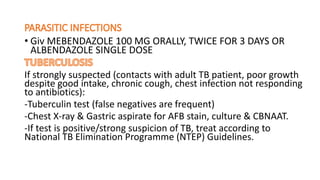
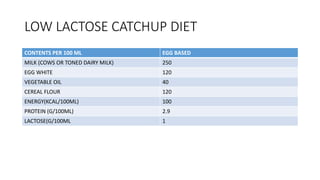
- Treatment depends on presence of medical complications, and involves therapeutic feeding to rehabilitate nutritional status.