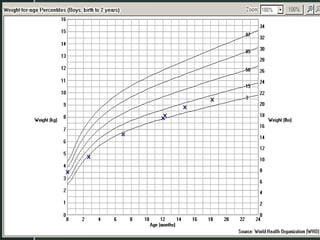
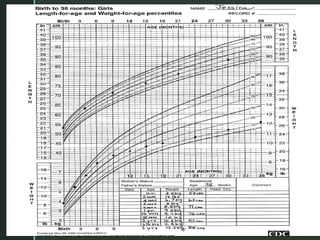
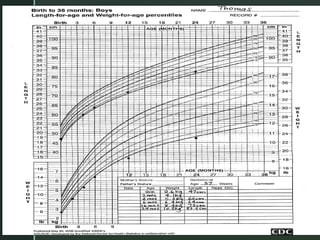
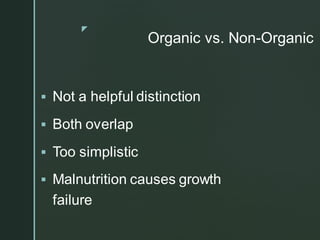
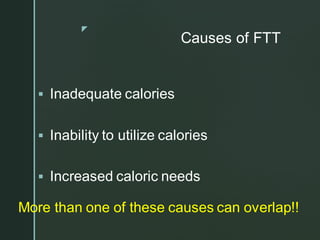
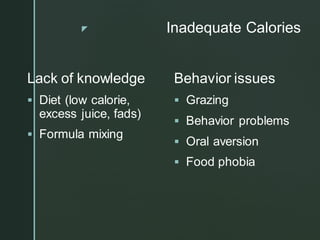
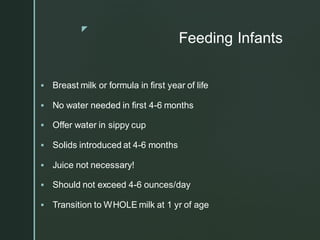
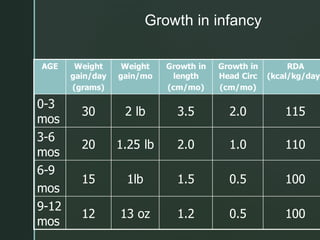
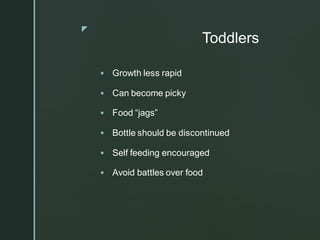
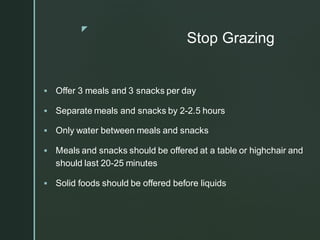
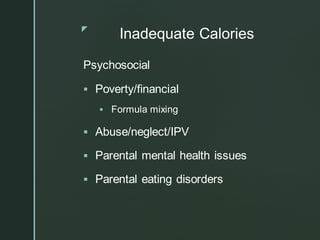
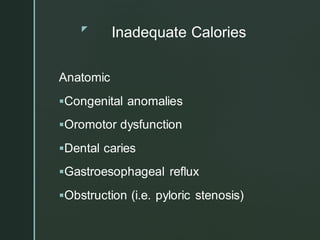
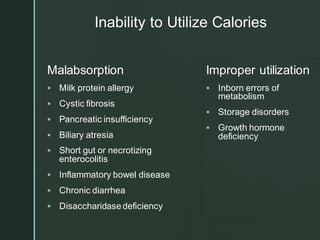
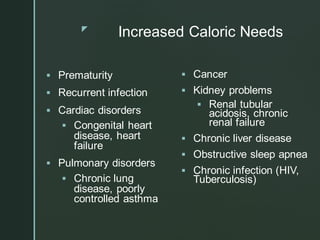
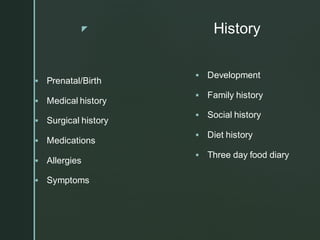
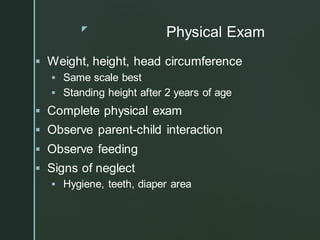
Failure to thrive (FTT) is a significant issue in pediatric care, affecting 1-5% of hospital referrals and often goes underdiagnosed. It is characterized by inadequate nutrition leading to abnormal growth patterns, with potential causes including inadequate calorie intake, inability to utilize calories, and increased caloric needs. Proper evaluation and treatment require a multidisciplinary approach, focusing on dietary changes, behavioral modifications, and consideration of underlying medical or social issues.