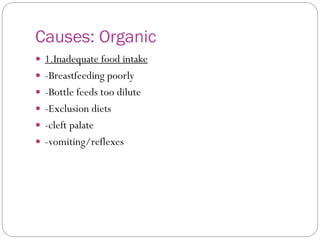
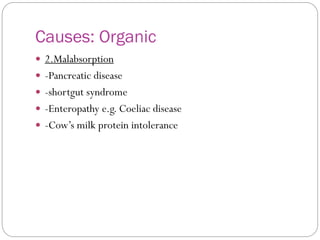
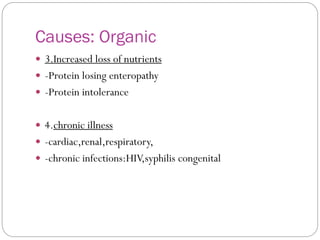
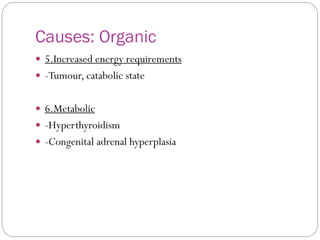
Failure to thrive is defined as inadequate weight gain or growth in infants and children. It can be caused by organic/medical factors that impair nutrition, such as malabsorption, or non-organic/psychosocial factors like neglect. Diagnosis involves assessing growth charts, dietary history, physical exam, and lab tests. Treatment focuses on providing adequate nutrition through diet and addressing any underlying medical or psychosocial issues impacting care and growth.