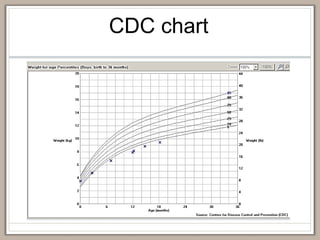
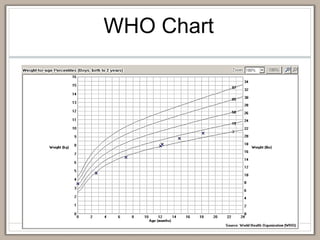
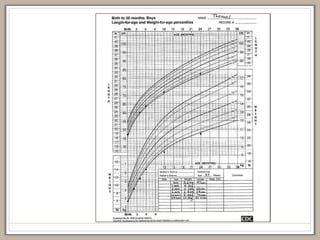
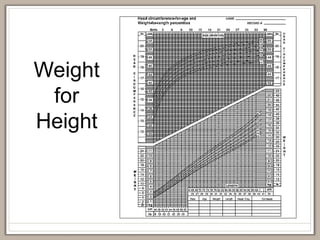
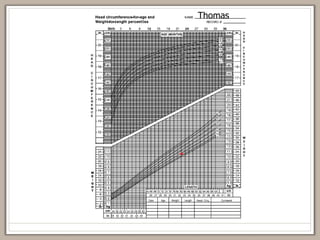
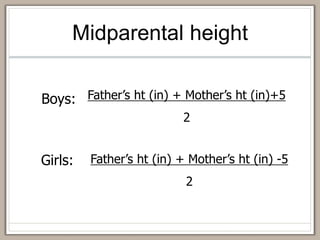
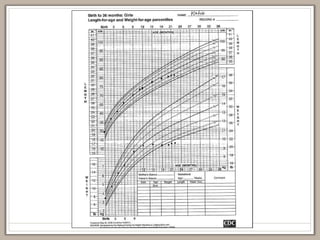
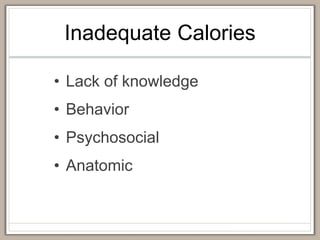
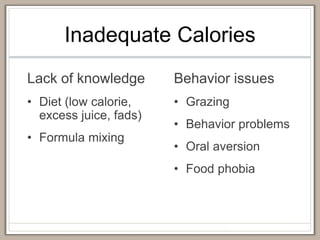
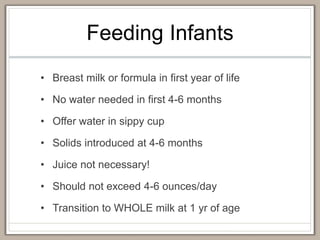
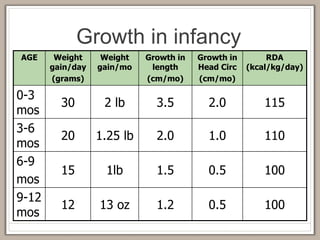
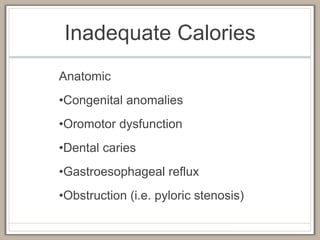
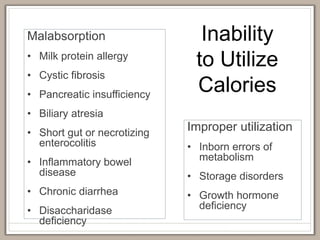
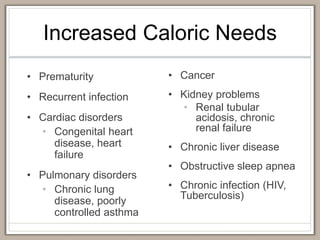
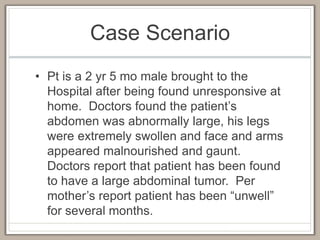
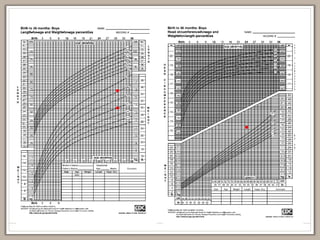
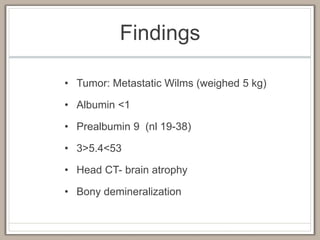
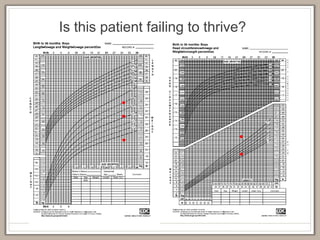
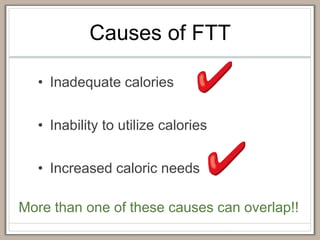
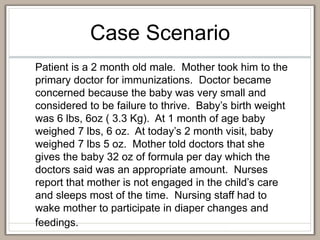
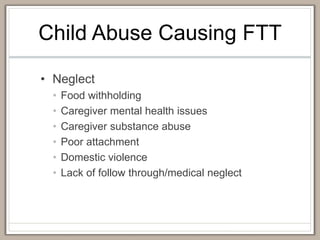
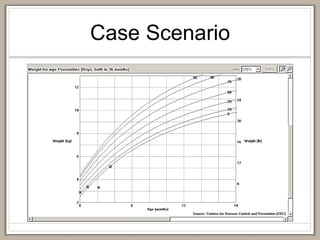
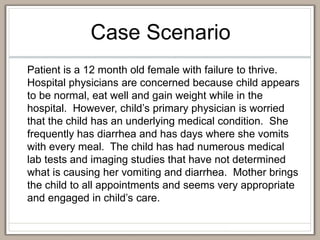
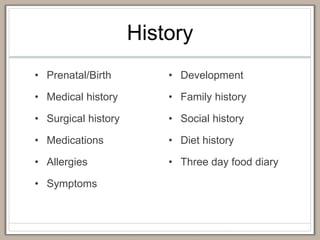
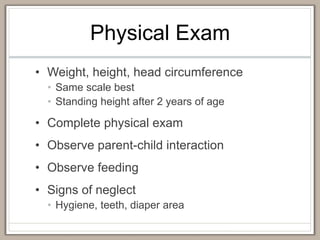
This document discusses failure to thrive in children. It begins by defining failure to thrive as inadequate nutrition leading to abnormal growth. Growth charts are then reviewed as tools to identify failure to thrive. The causes of failure to thrive are categorized as inadequate calories, inability to utilize calories, and increased caloric needs. Child abuse, including neglect, medical child abuse, and physical/sexual abuse, are also discussed as potential causes. The evaluation, treatment, and multidisciplinary management of failure to thrive are outlined.