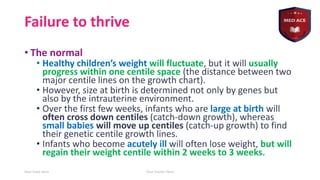
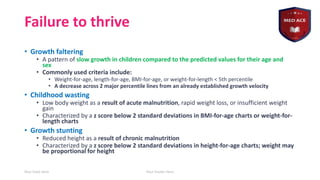
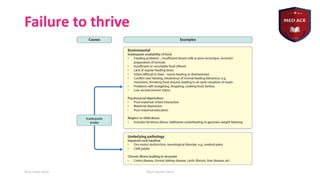
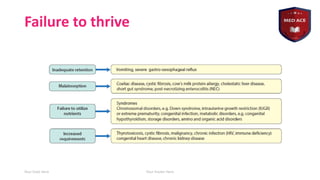
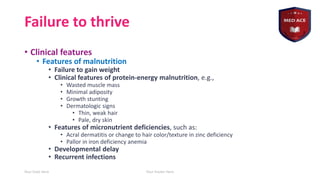
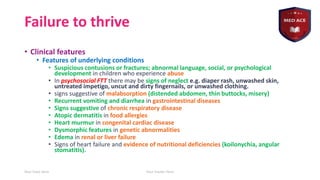
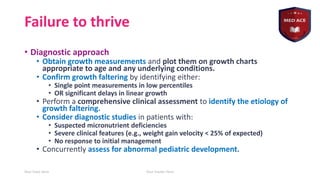
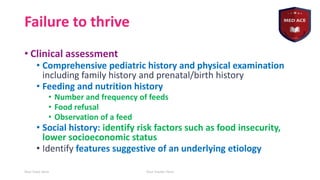
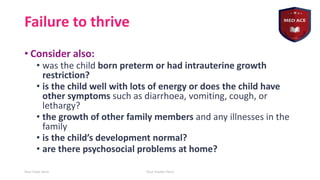
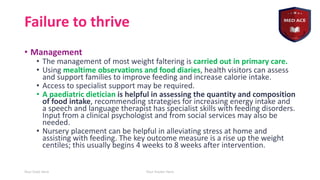
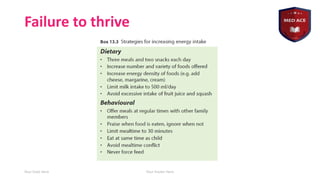
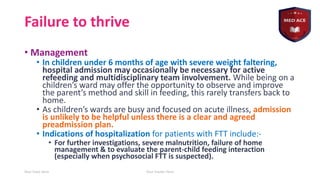
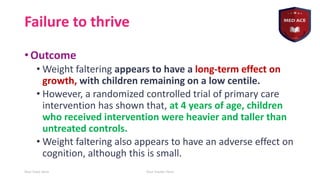
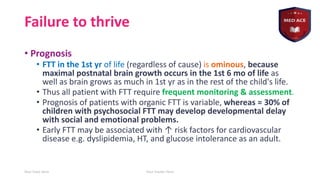
The document discusses 'failure to thrive' in children, identifying it as a pattern of slow growth compared to expected values for age and gender, and outlines criteria for diagnosis and clinical features. It emphasizes the importance of comprehensive assessments to identify underlying causes and describes management strategies, including dietary interventions and potential hospitalization. The document also highlights the long-term effects of weight faltering and the need for ongoing monitoring and support for affected children.