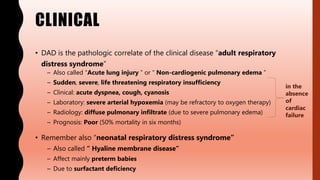
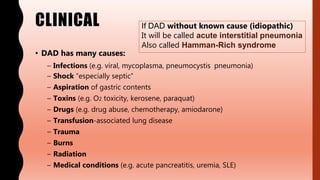
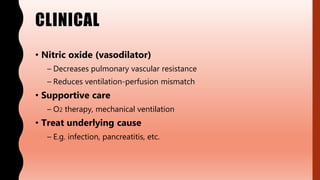
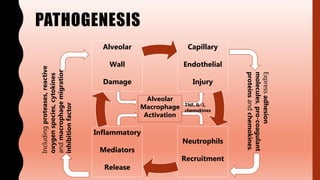
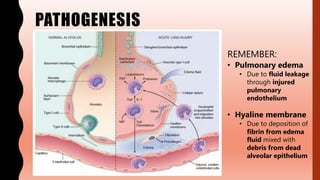
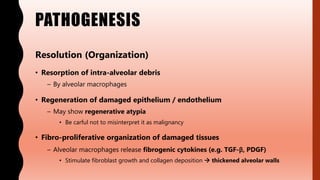
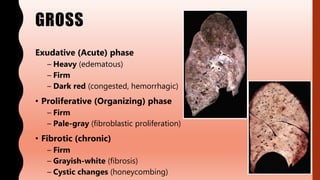
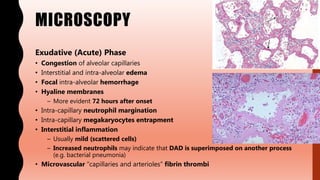
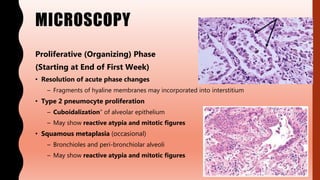
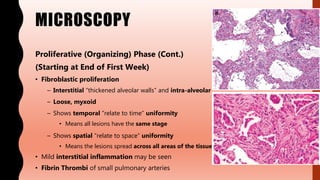
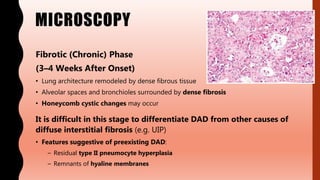
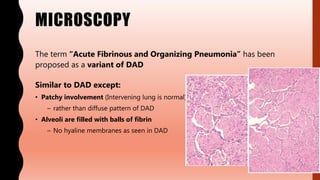
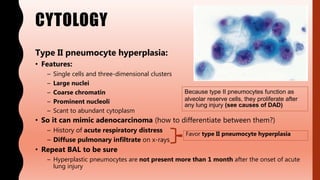
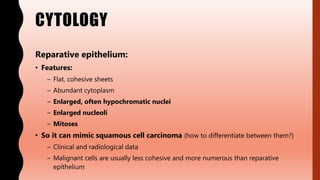
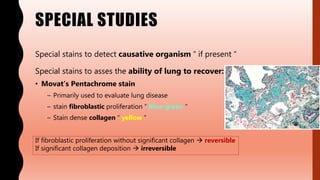
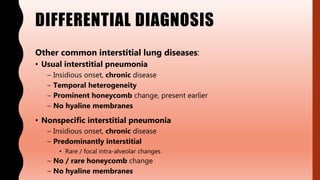
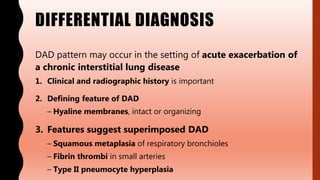
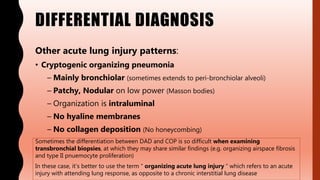
This document summarizes diffuse alveolar damage (DAD), the pathologic correlate of acute respiratory distress syndrome. DAD is characterized by diffuse pulmonary edema, hyaline membrane formation, and poor prognosis. It has many causes including infections, shock, aspiration, and toxins. Pathologically, DAD involves capillary endothelial injury, neutrophil recruitment, alveolar wall damage, and pulmonary edema. The condition progresses from an exudative to proliferative and fibrotic phase as the lungs attempt to heal. Special stains are used to identify causative organisms and assess lung recovery potential. DAD must be differentiated from other interstitial lung diseases and acute lung injury patterns.