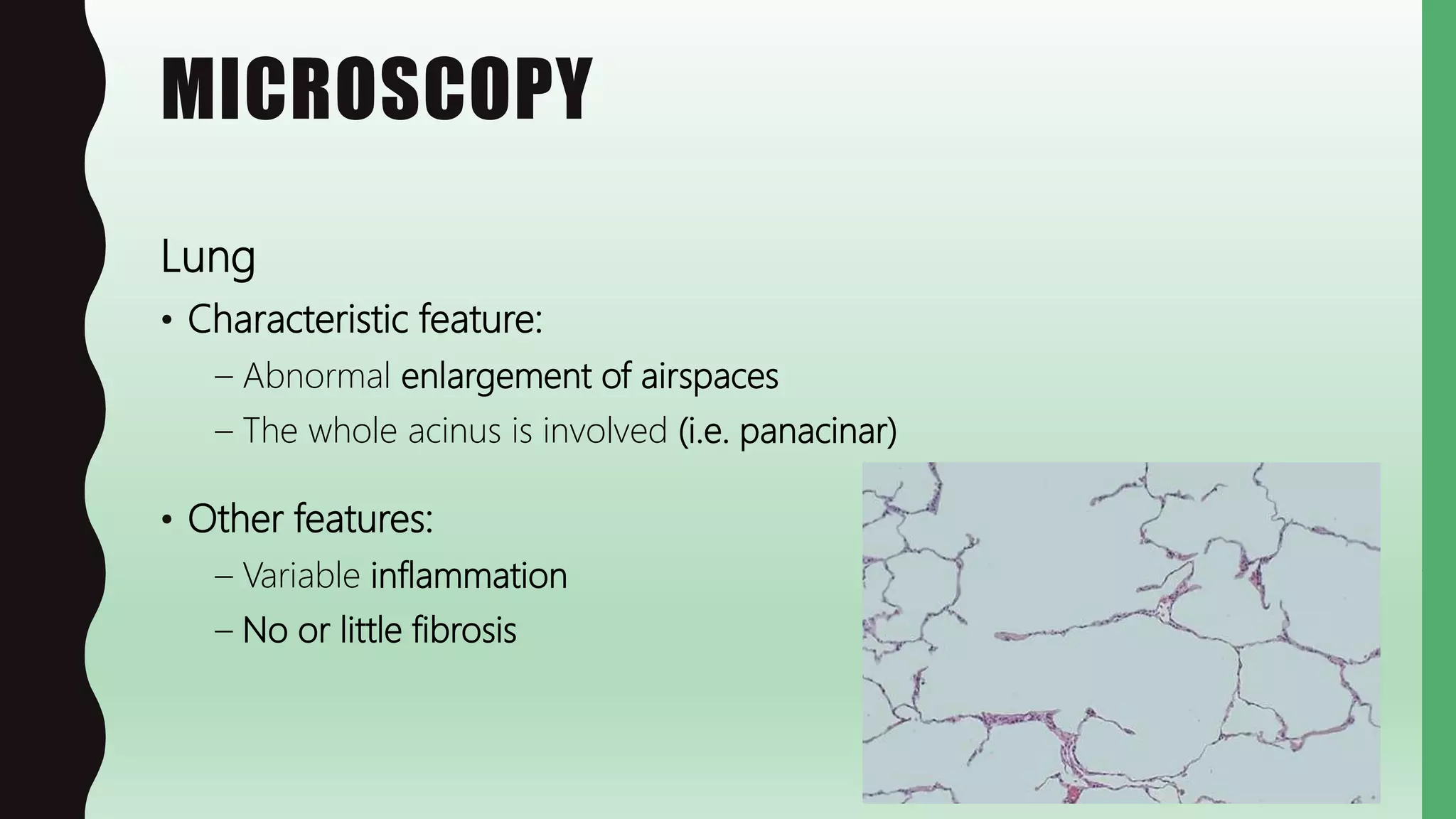
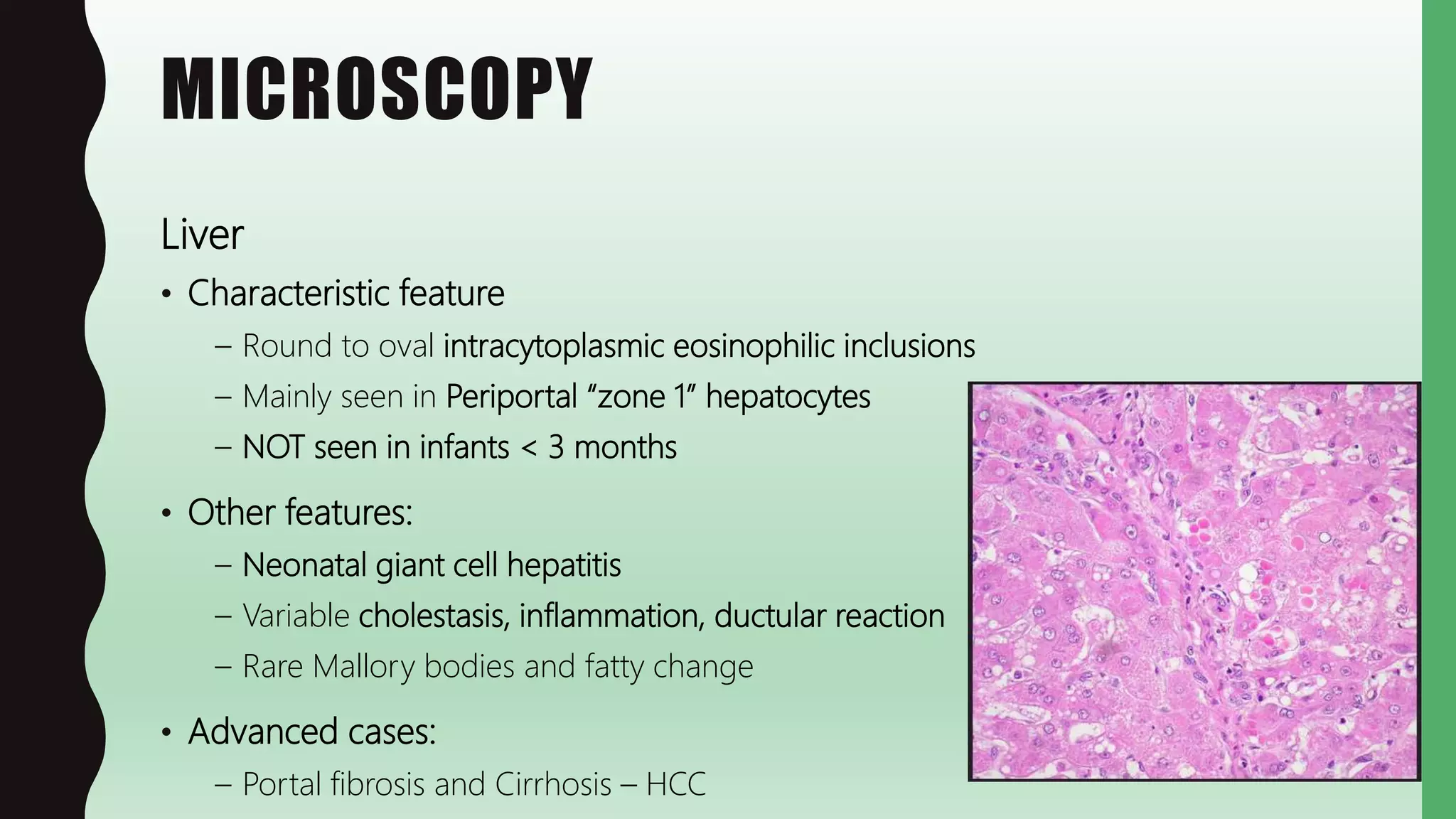
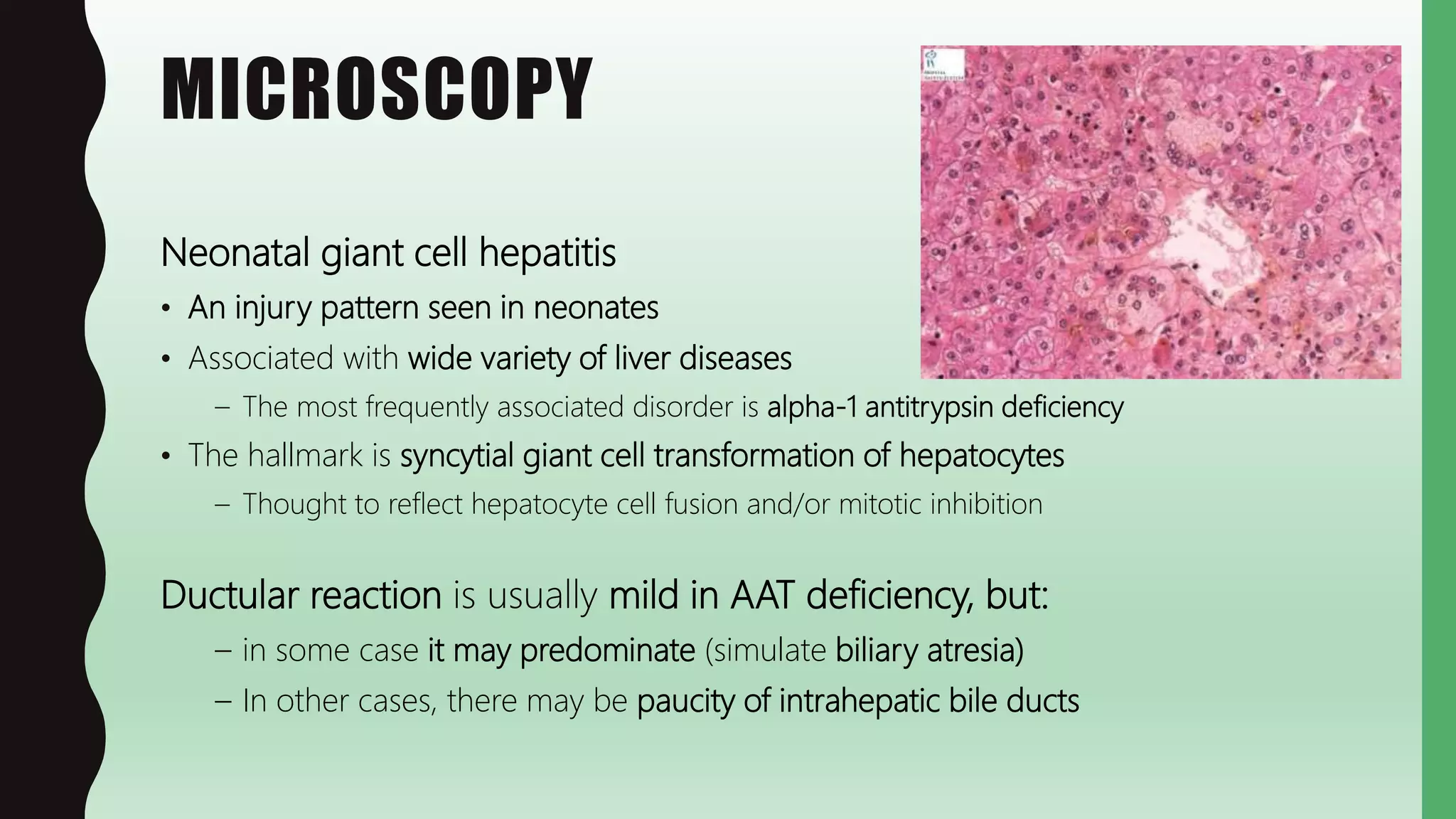
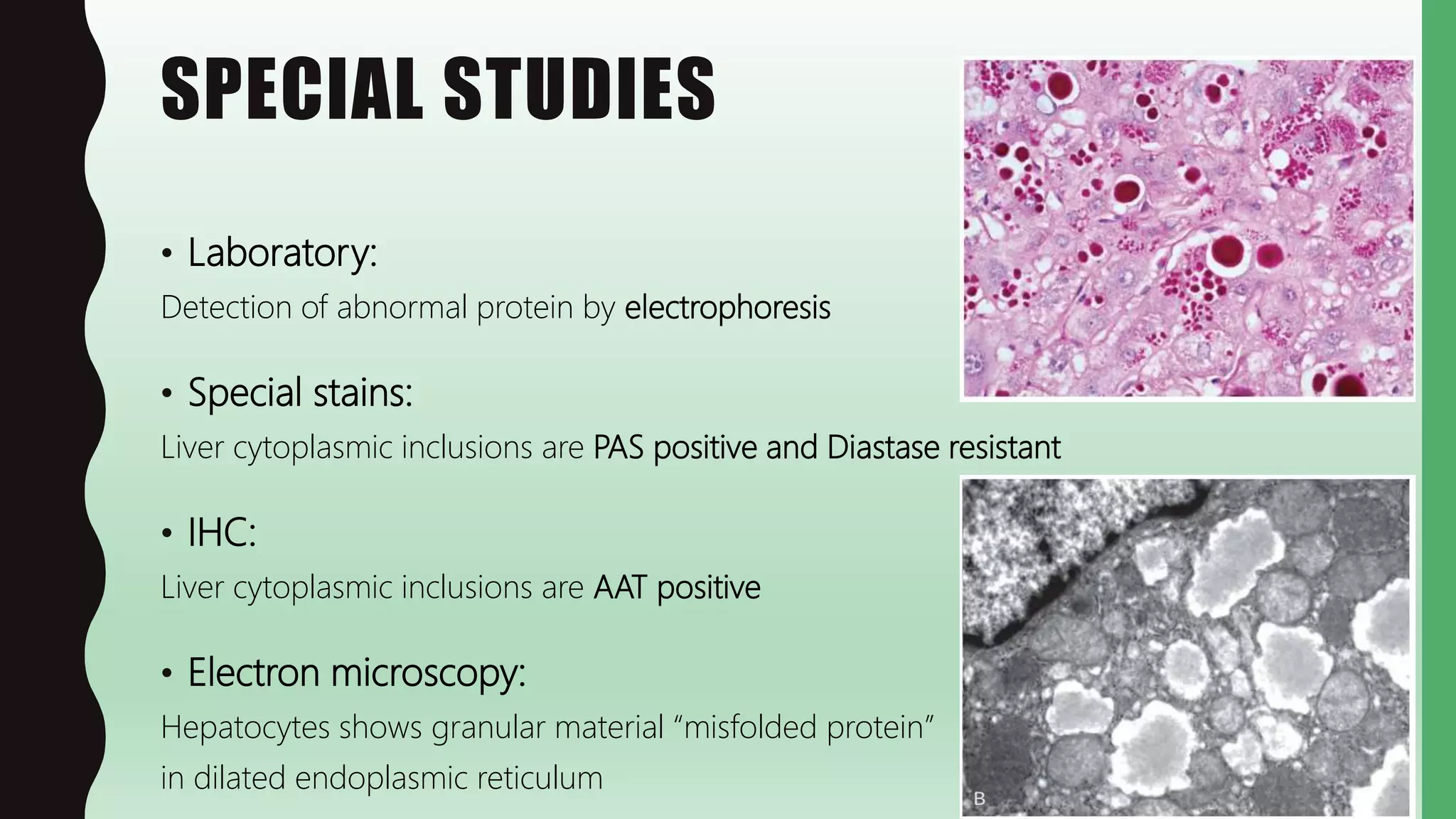
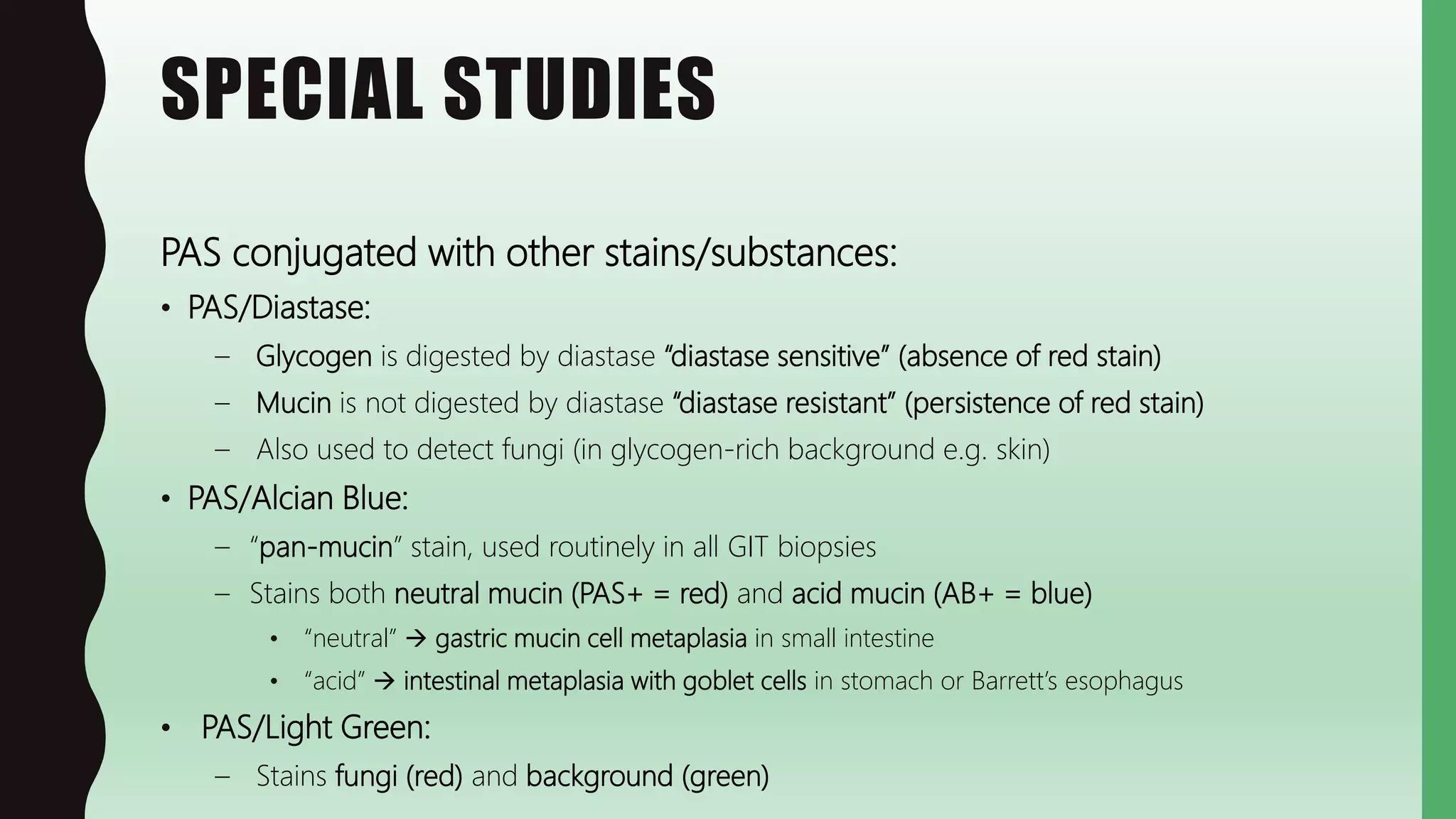
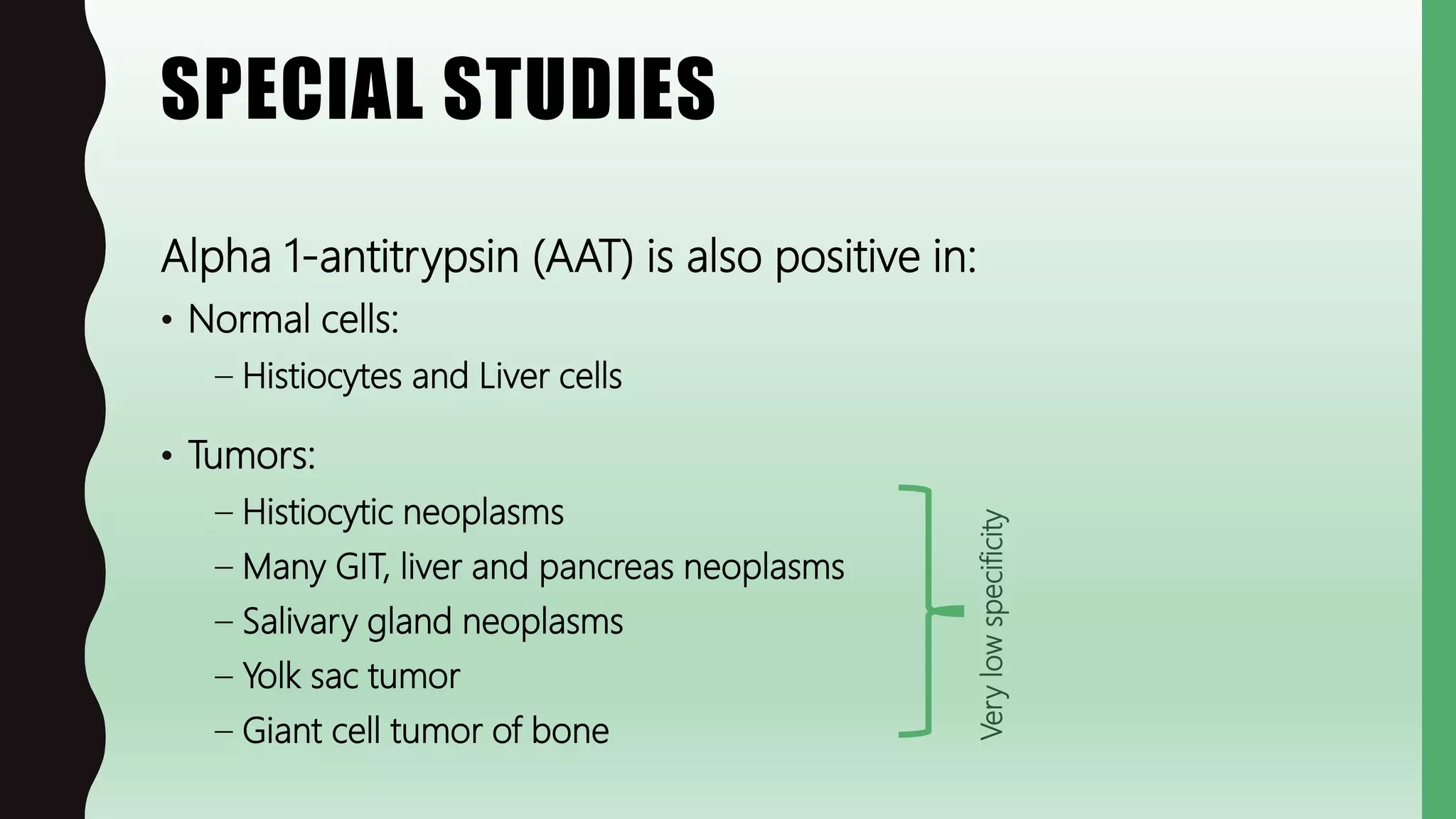
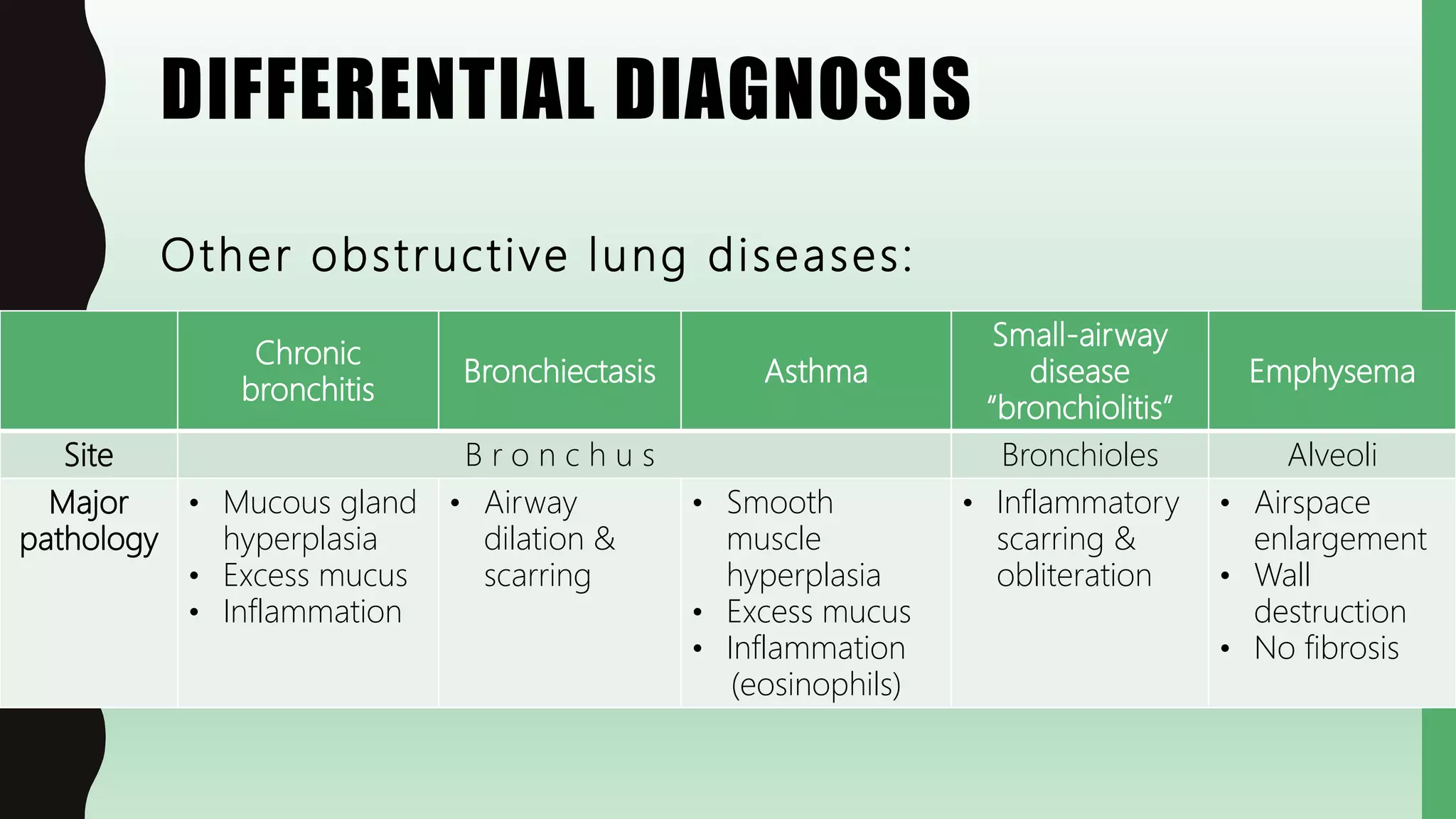
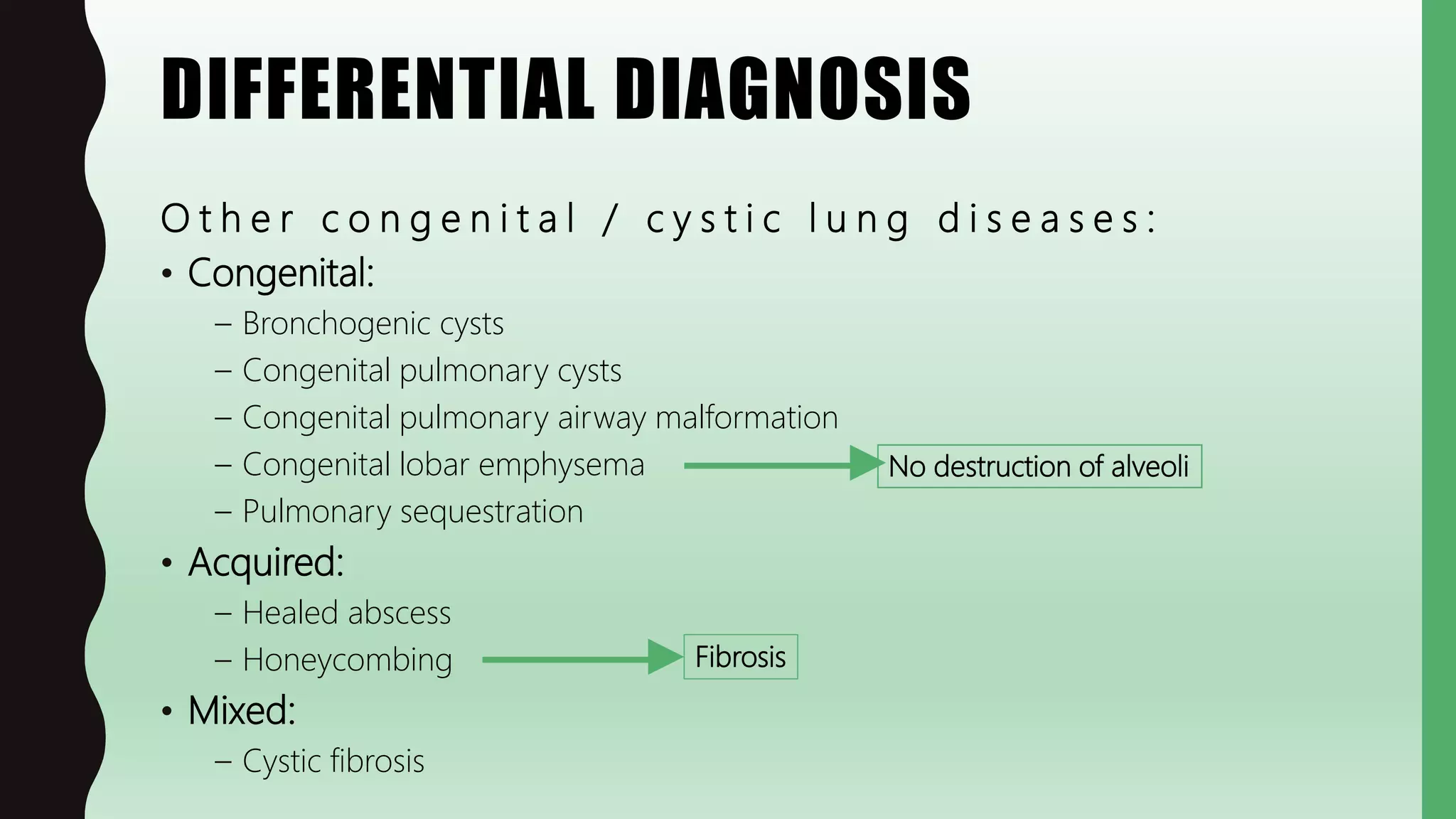
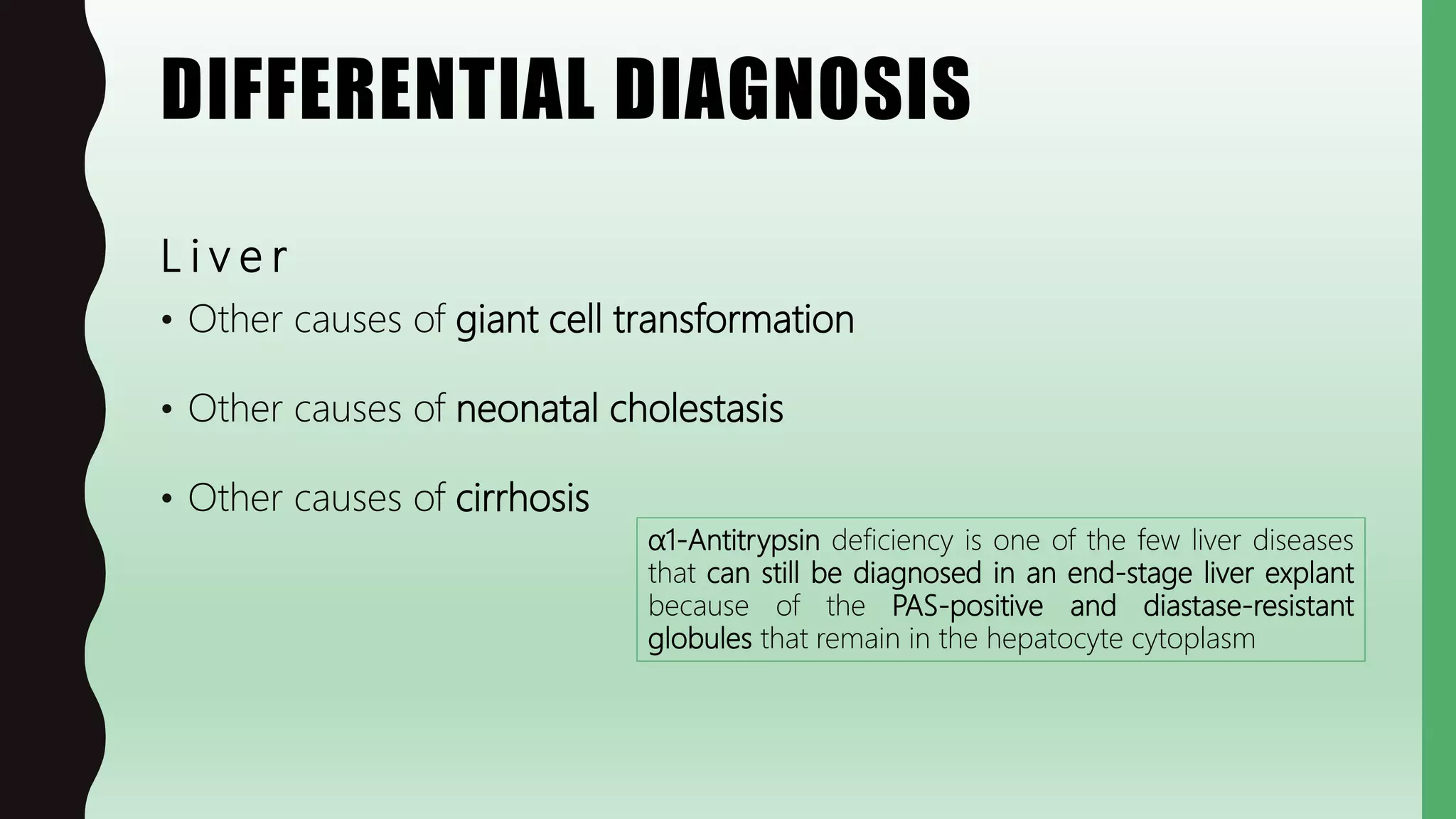
This document discusses alpha-1 antitrypsin deficiency. It is an autosomal recessive disease causing deficiency of alpha-1 antitrypsin (AAT), which normally inhibits neutrophil elastase. This leads to lung emphysema and liver disease. In the lung, AAT deficiency results in panacinar emphysema due to uncontrolled neutrophil elastase activity. In the liver, AAT accumulates in hepatocytes, seen as PAS+ diastase-resistant inclusions. The disease presents in childhood with liver disease such as neonatal hepatitis or later with lung emphysema. Treatment involves AAT augmentation therapy for the lung. The pathology, clinical features, genetics and pathogenesis are described.