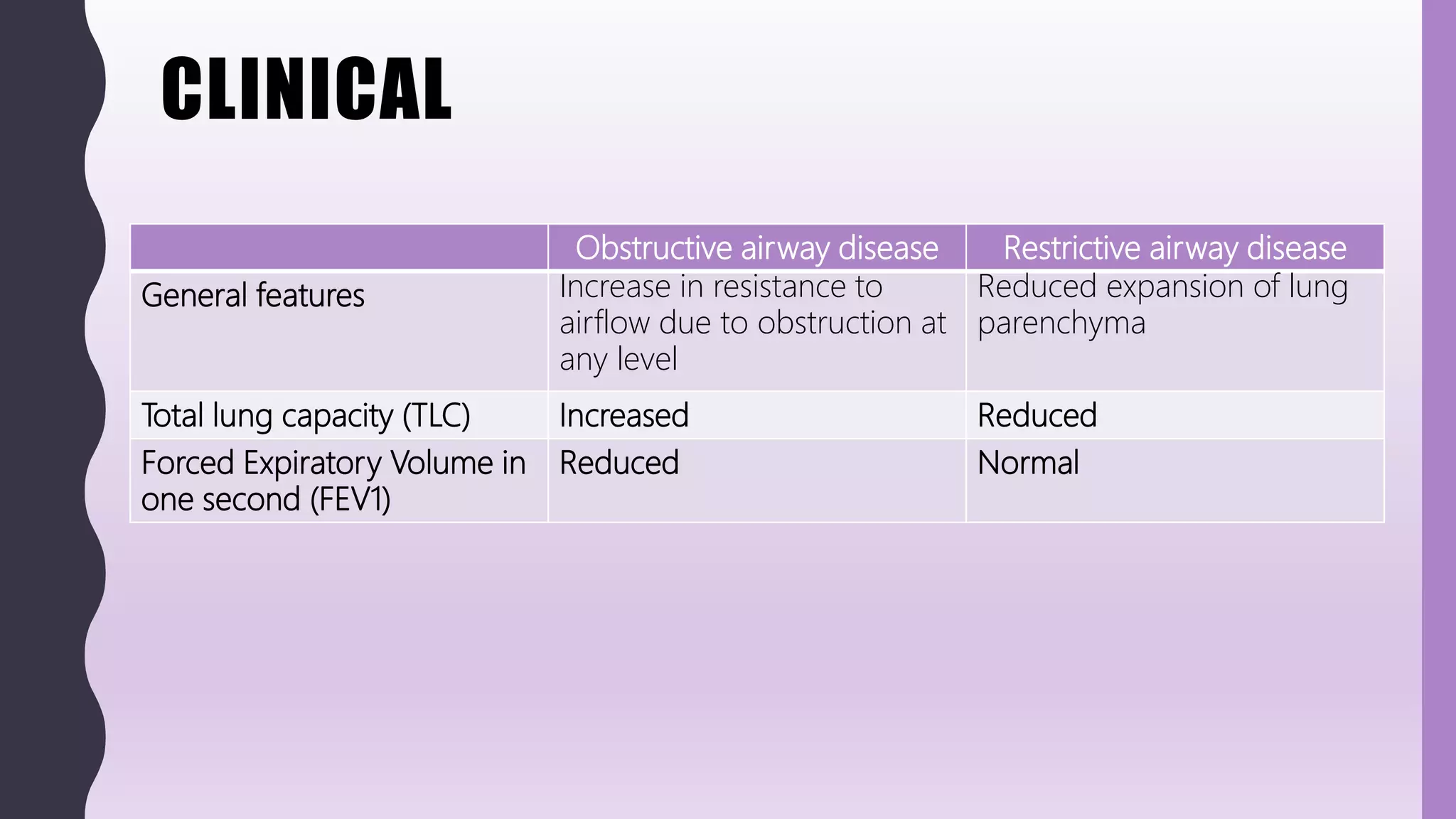
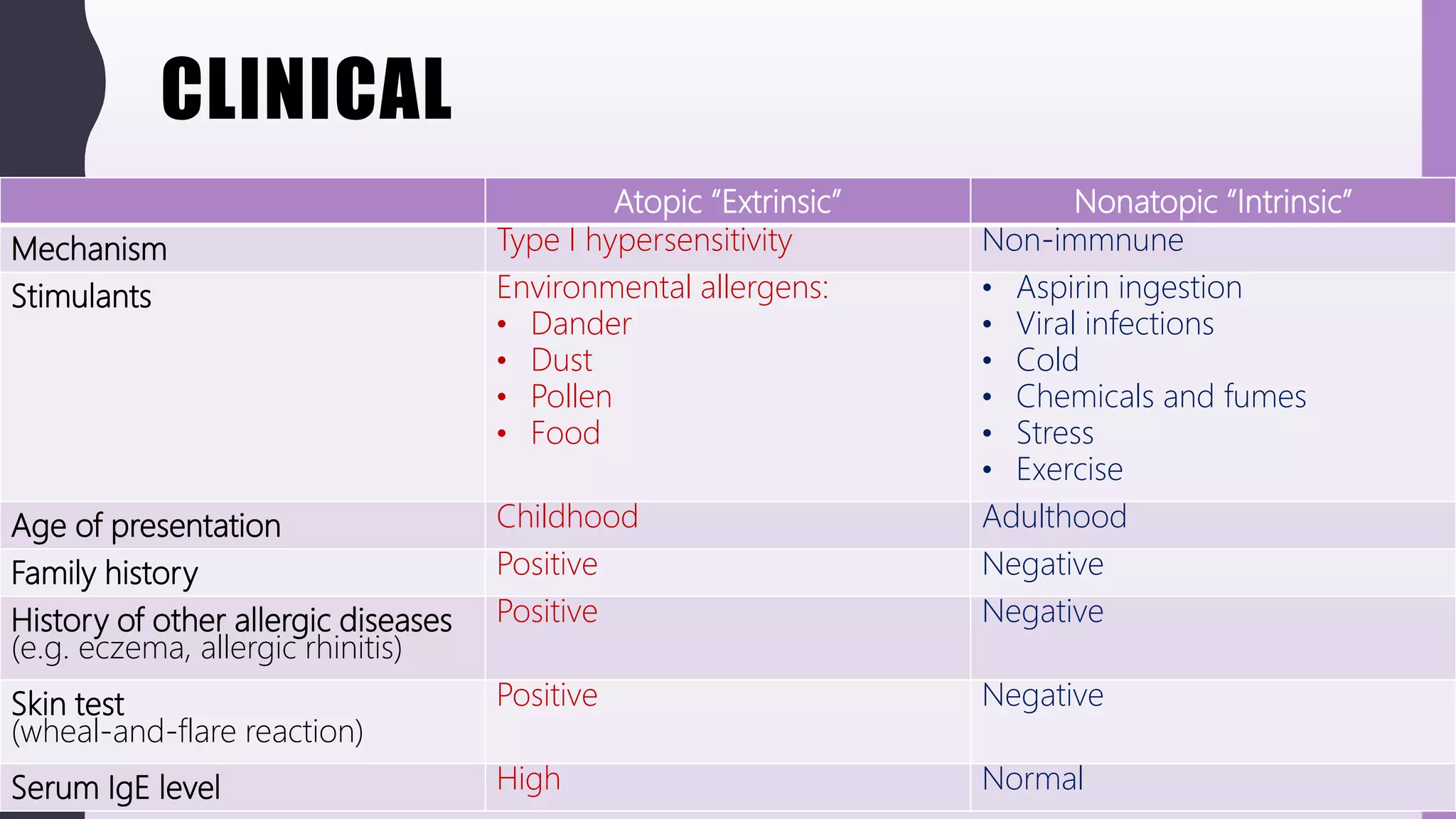
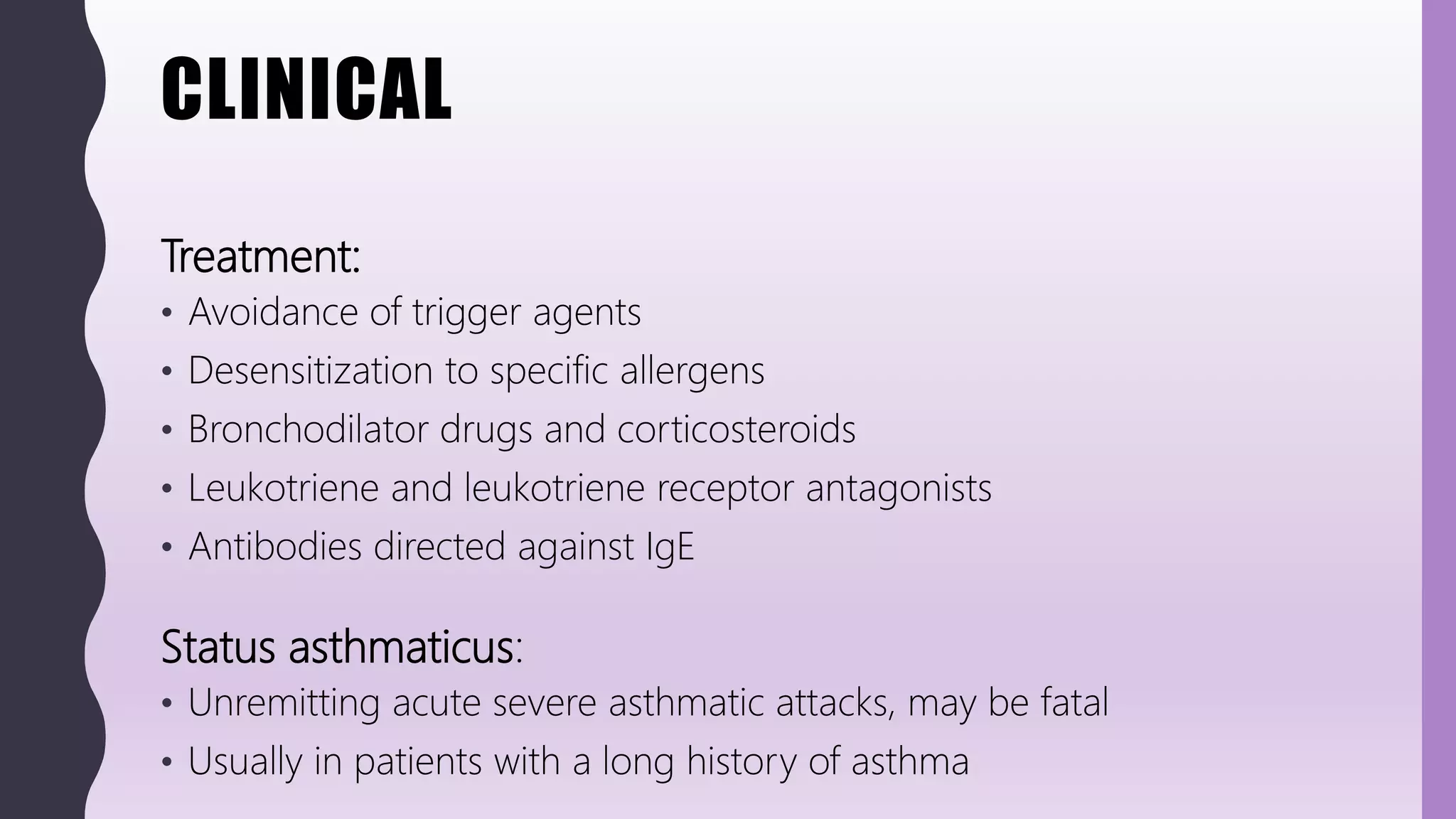
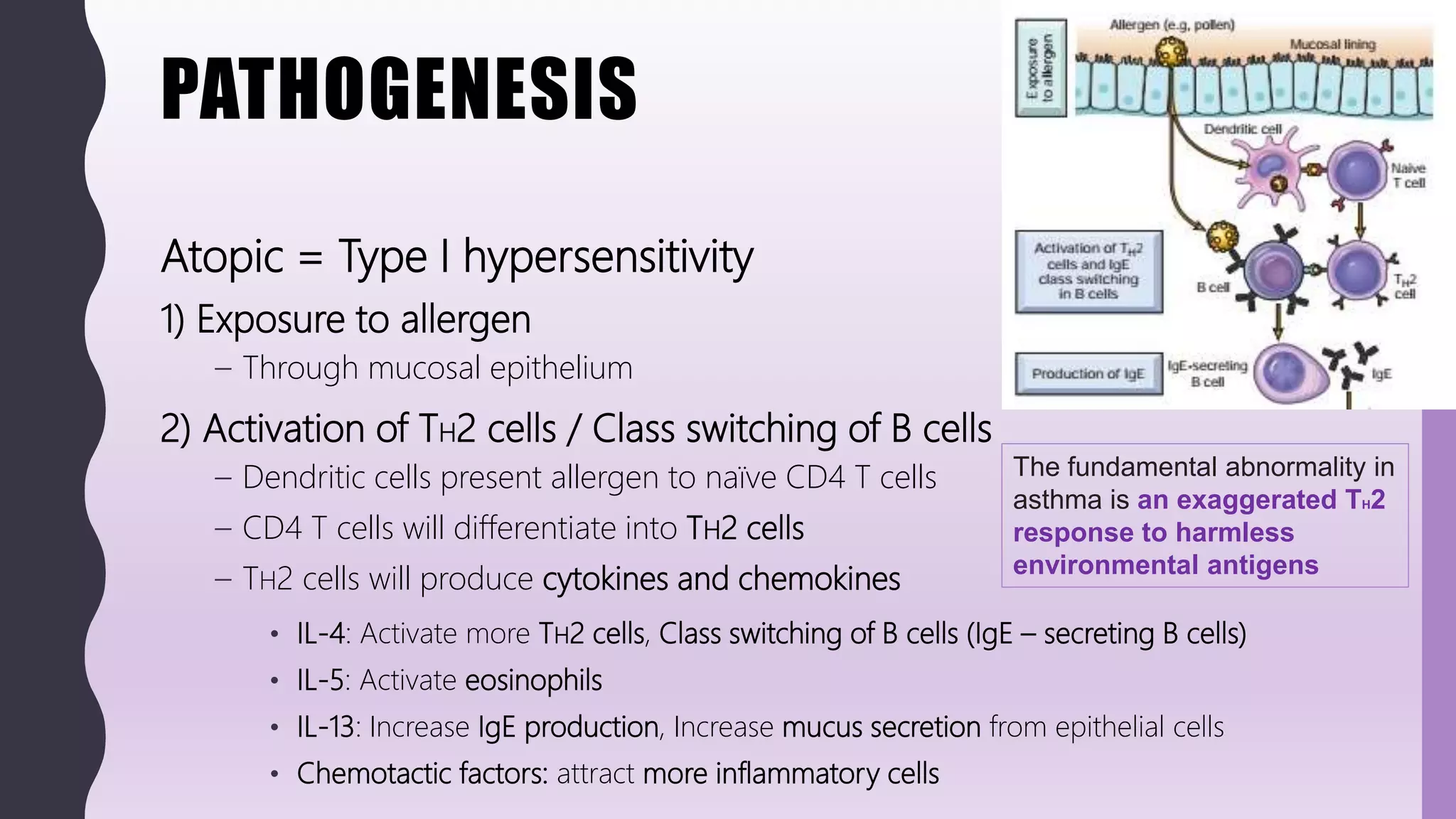
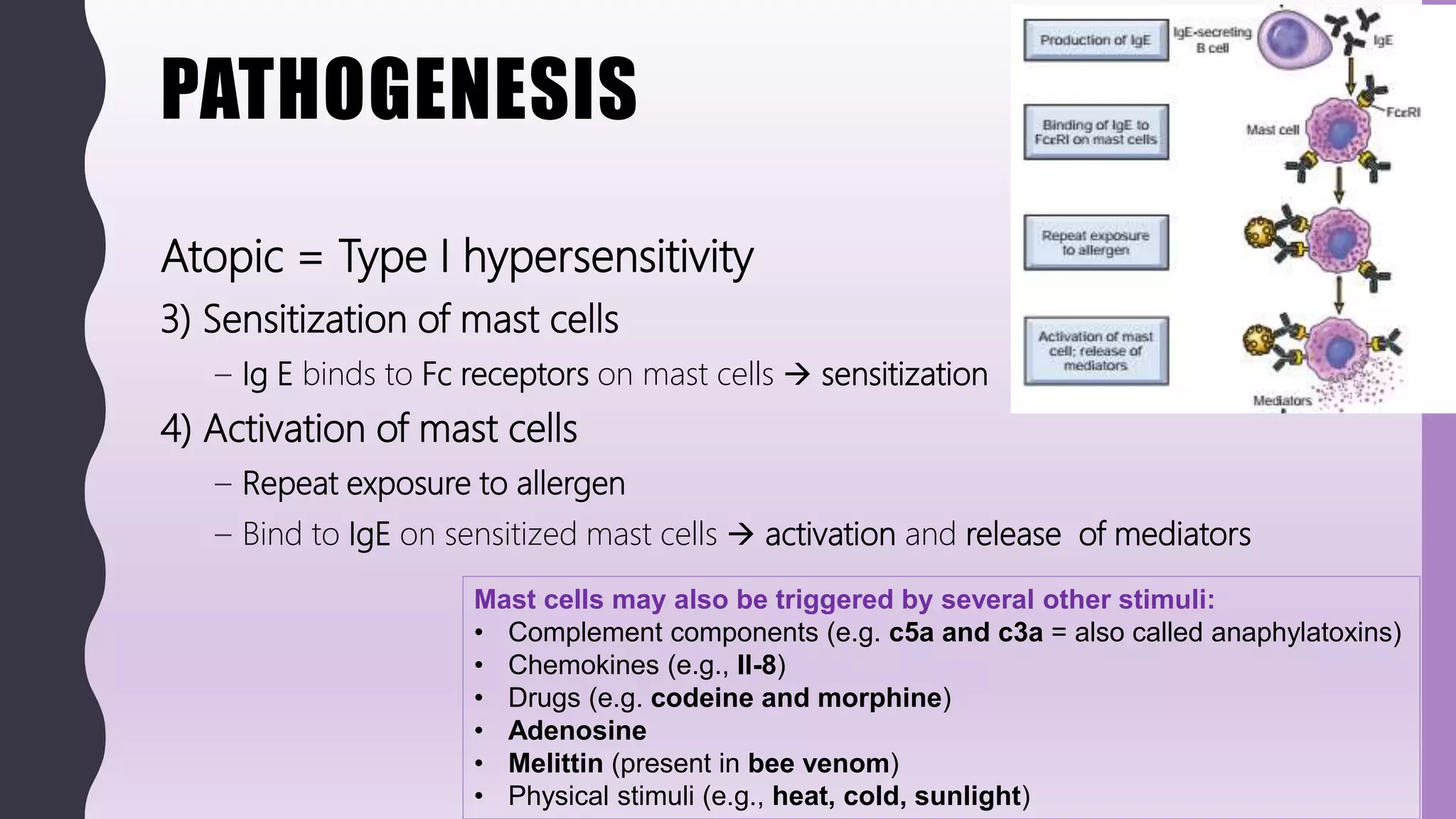
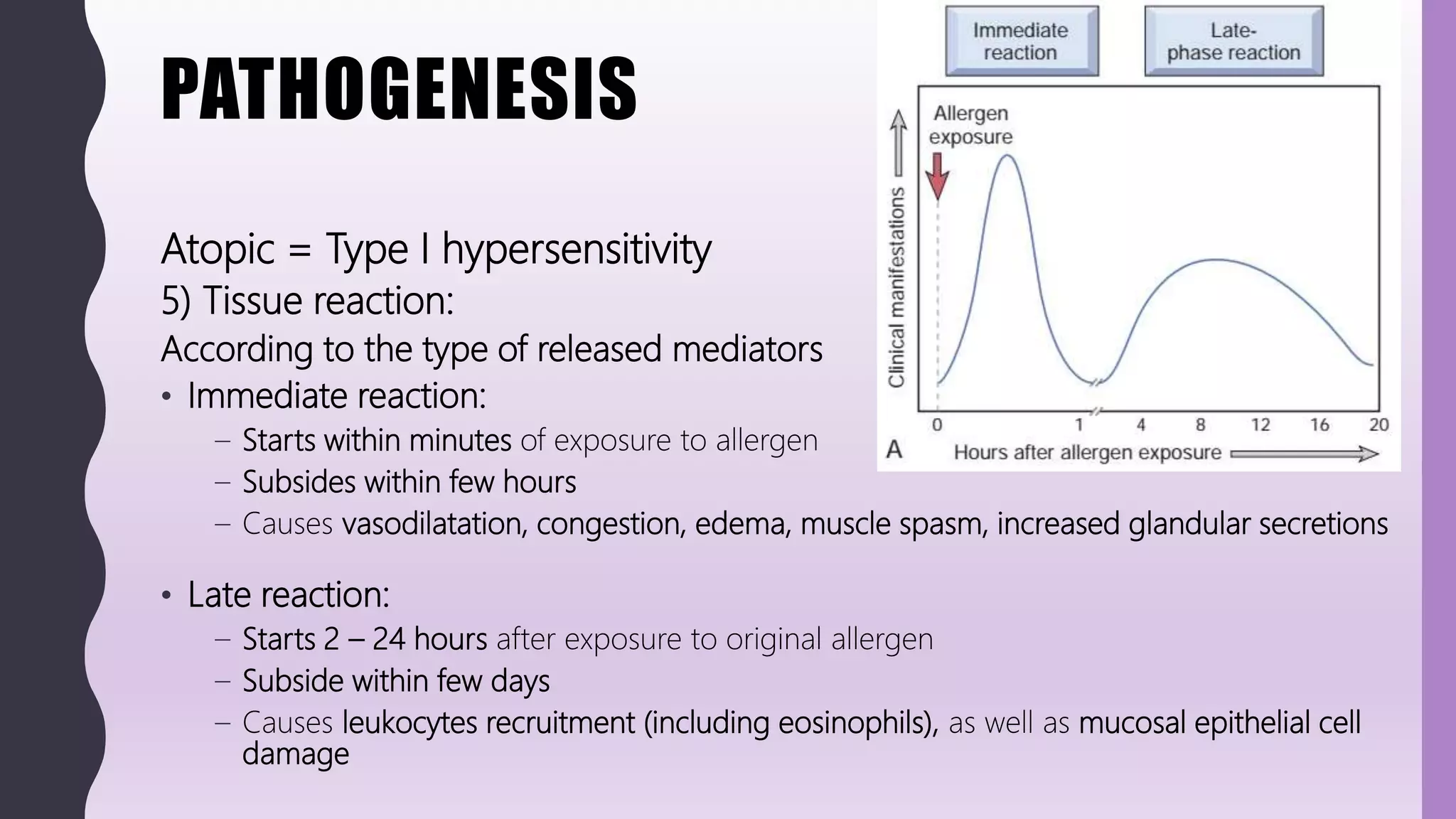
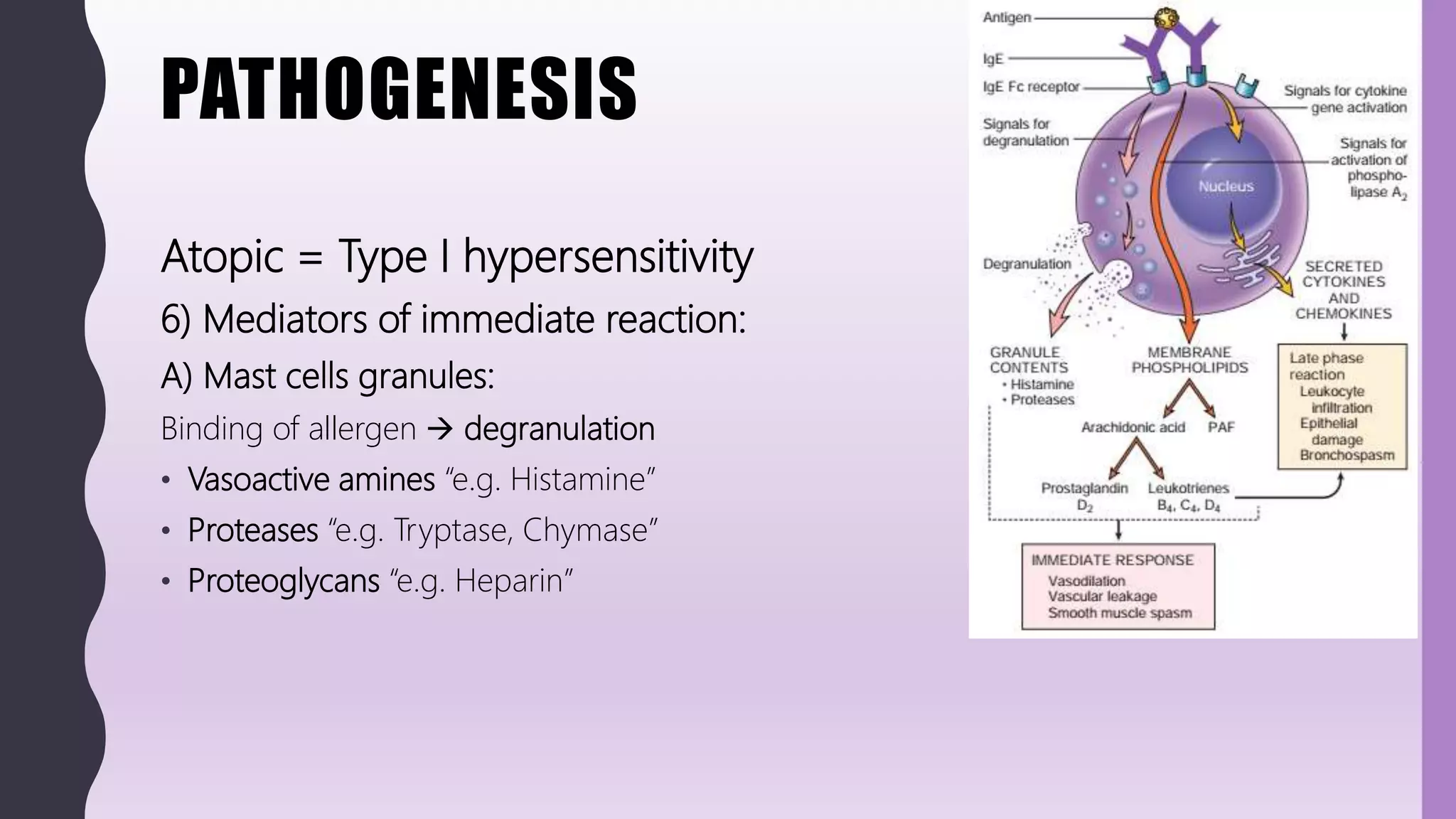
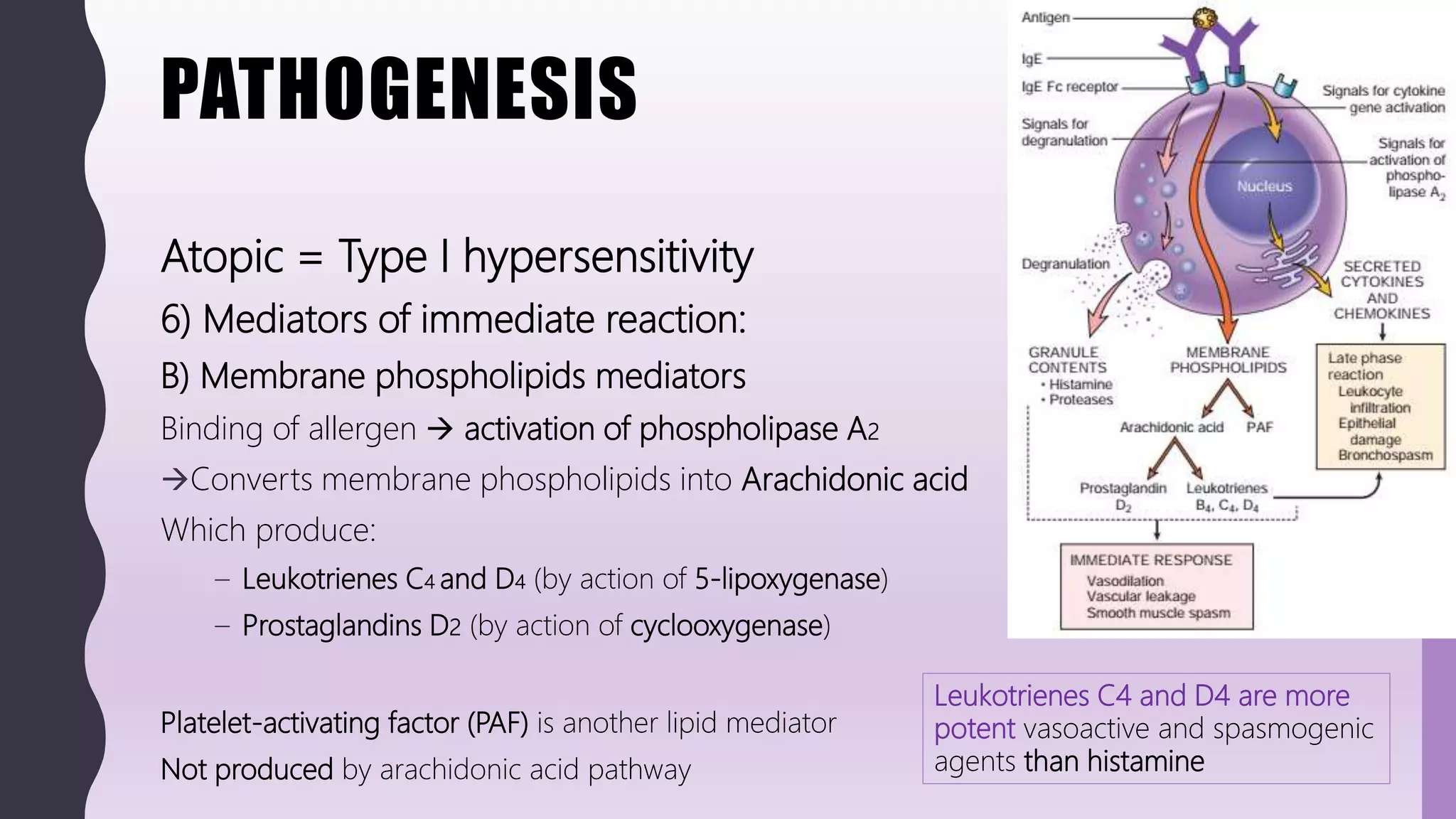
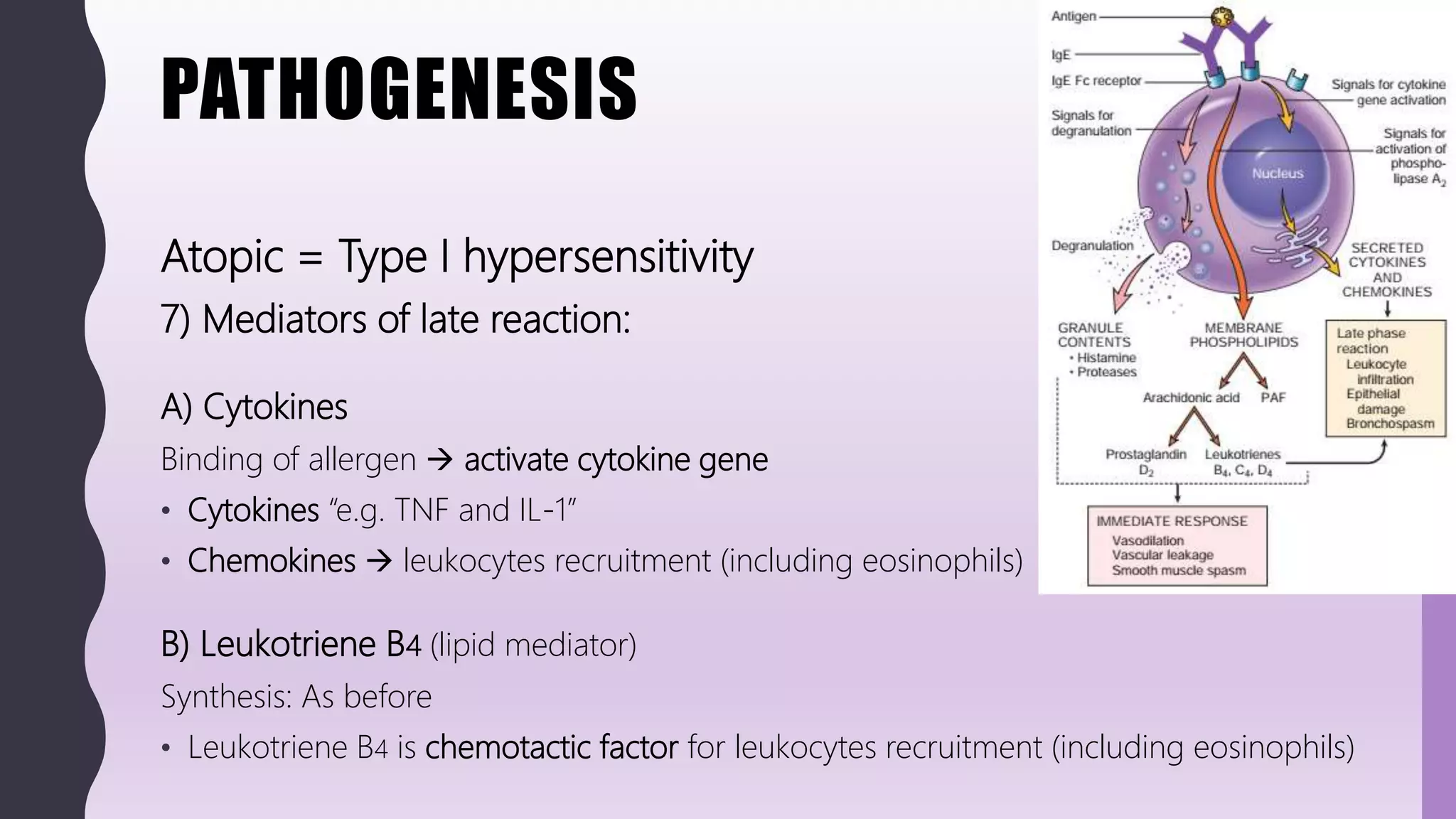
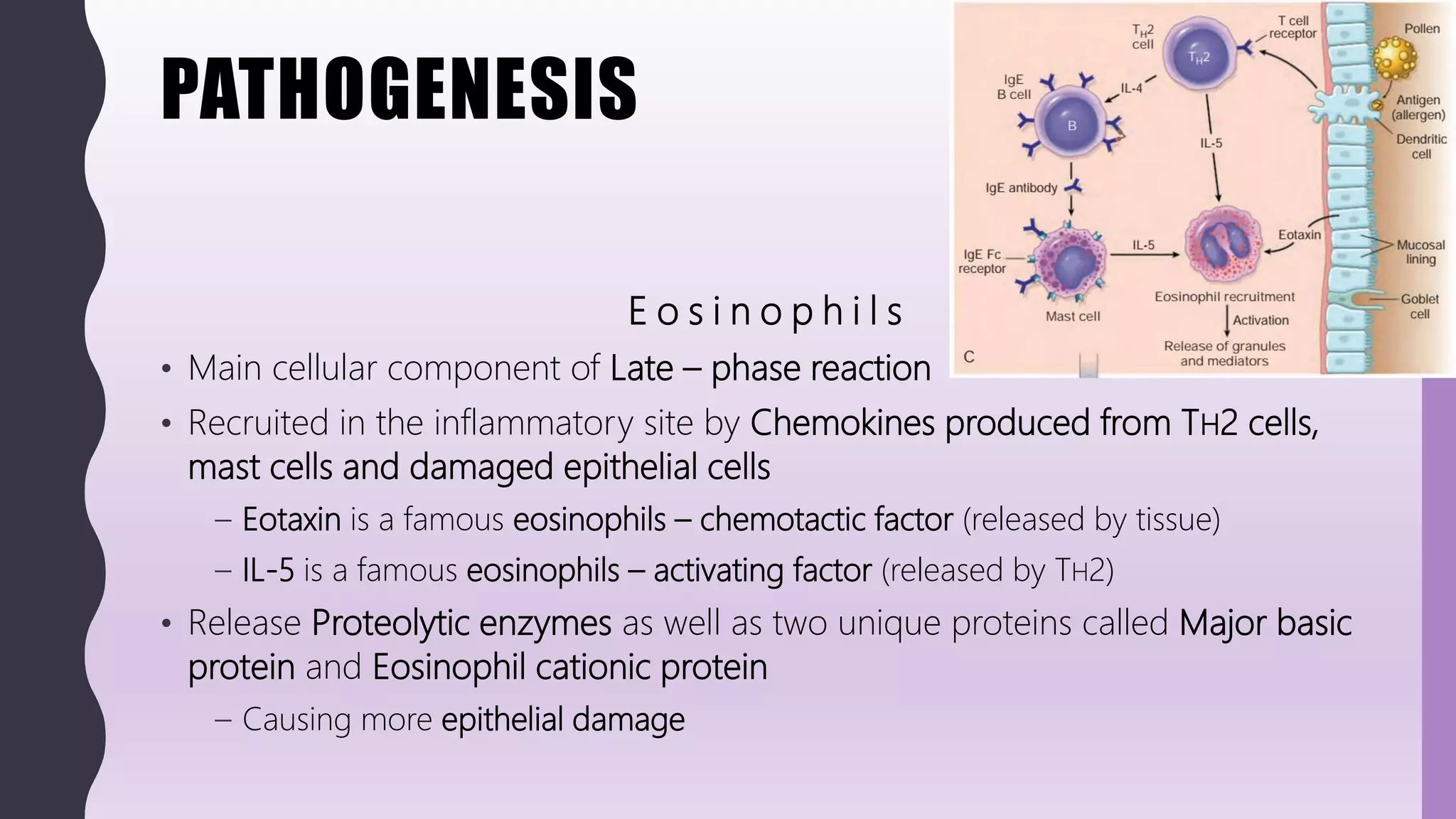
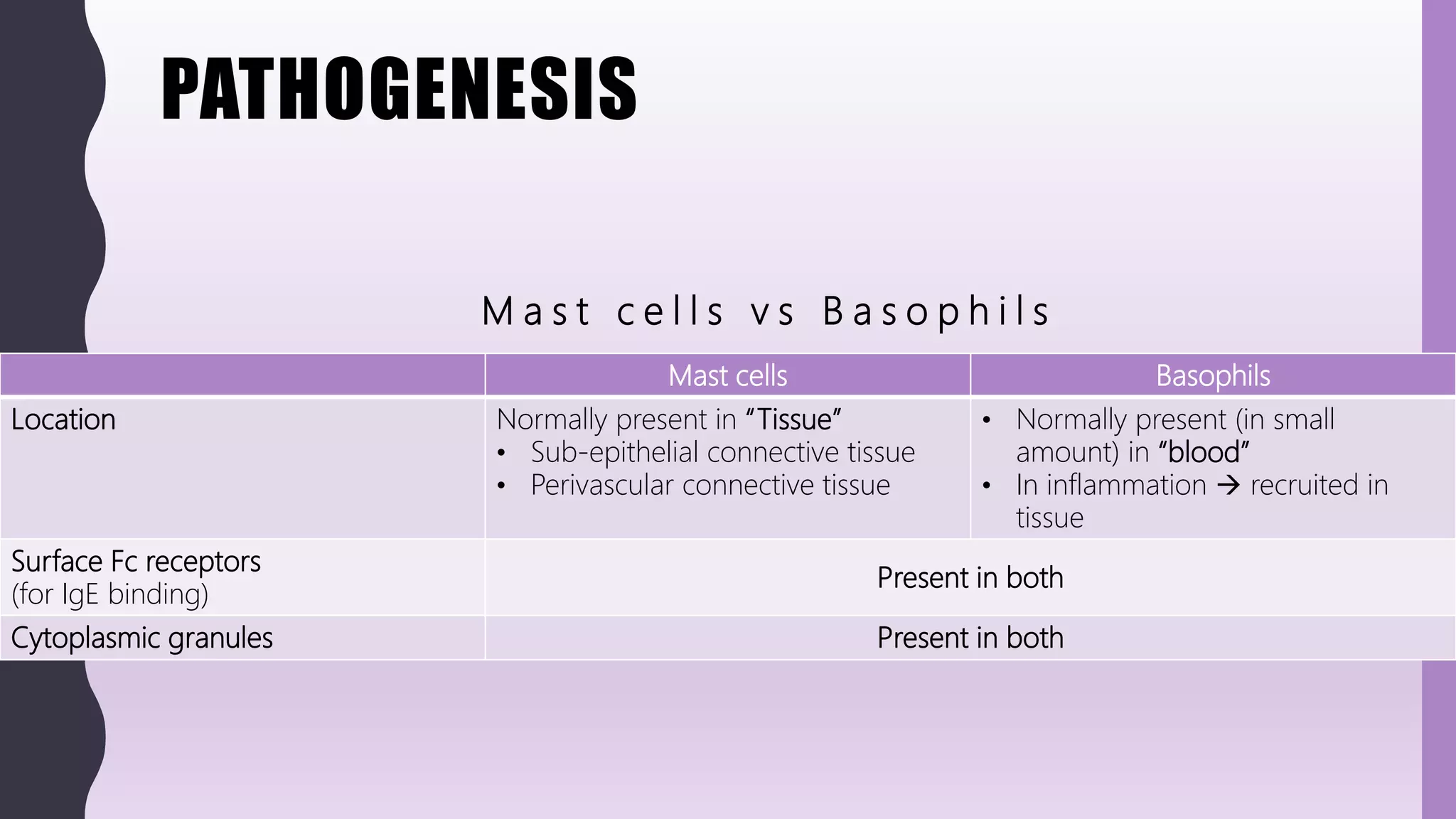
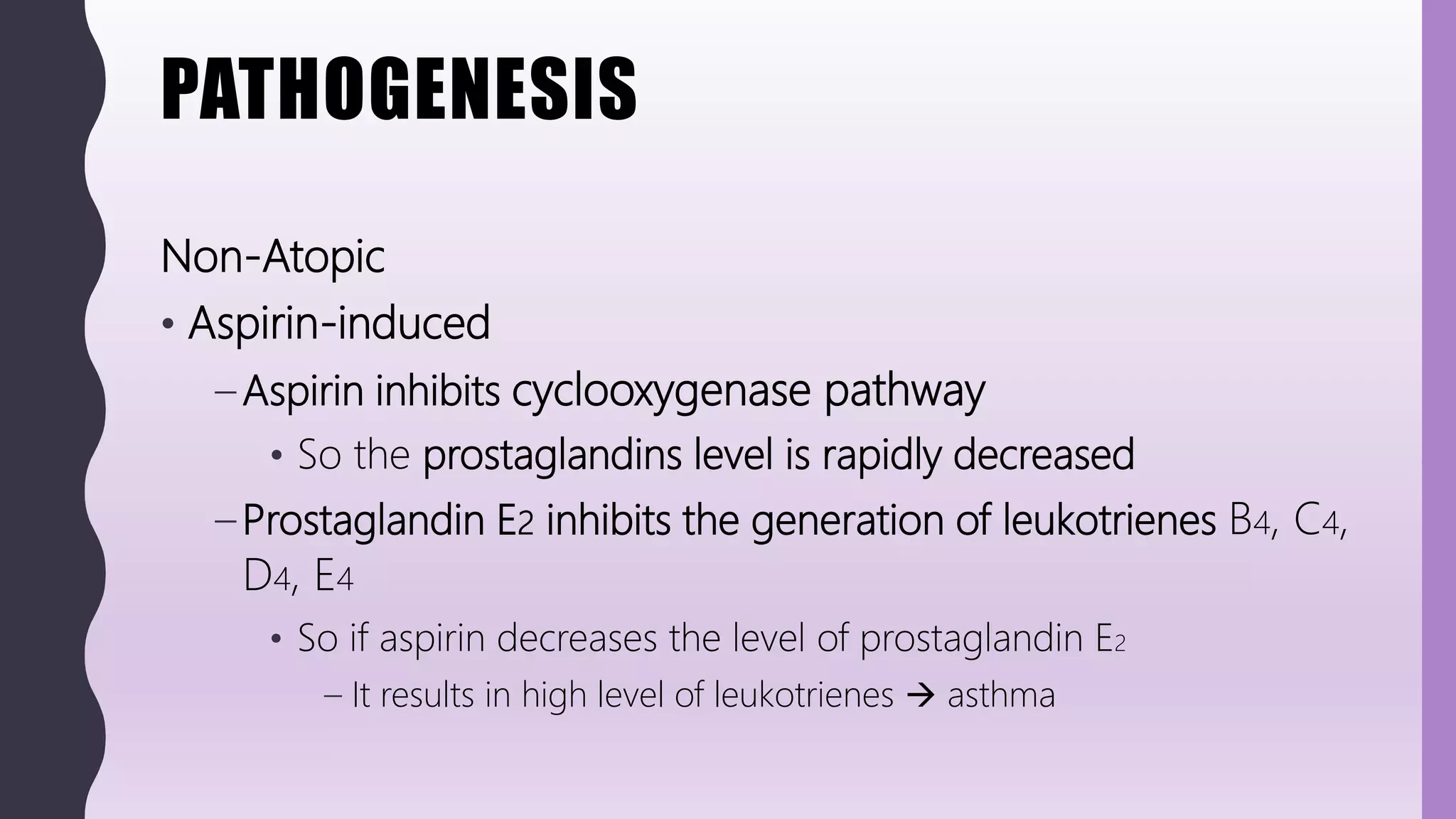
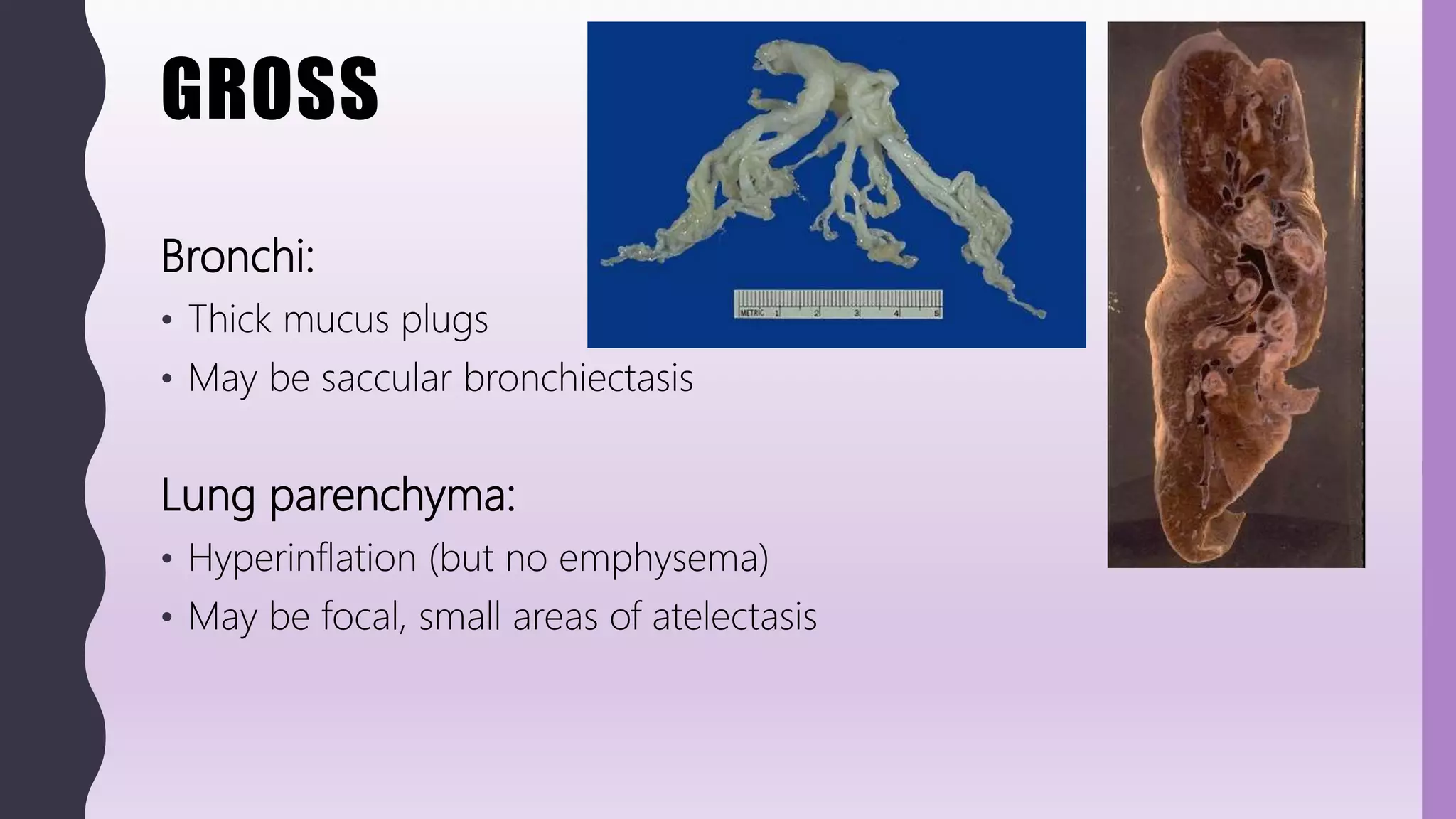
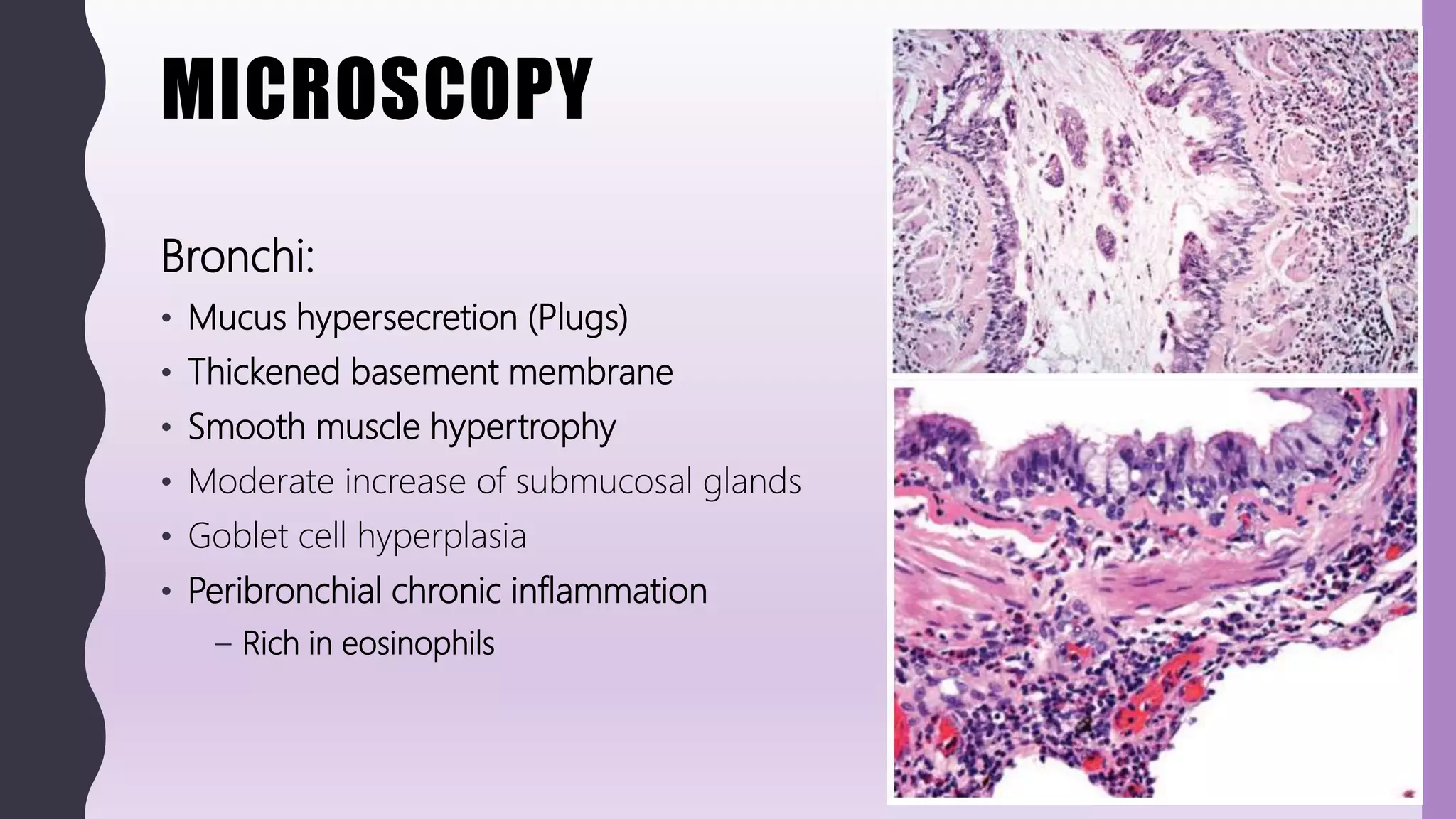
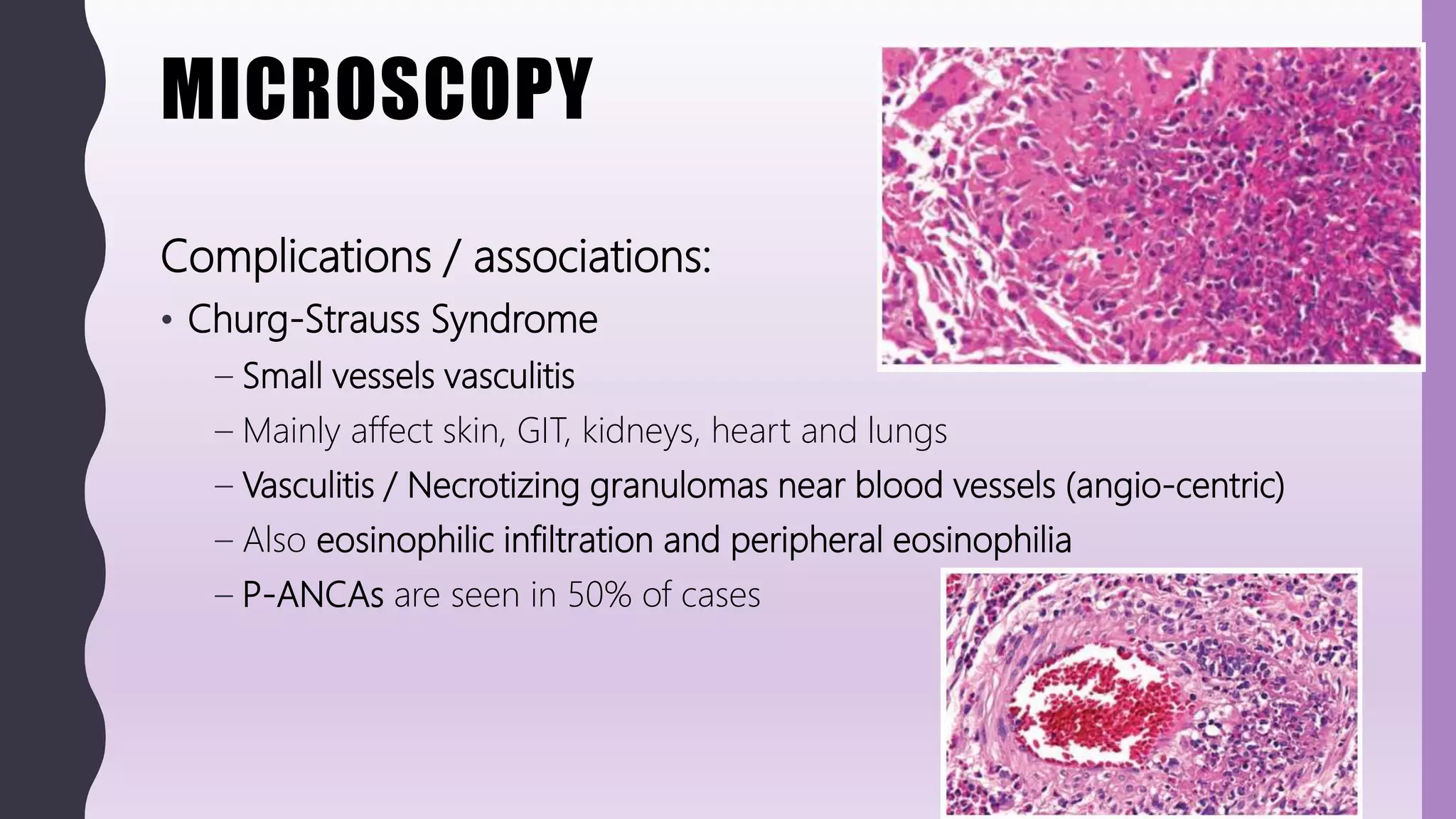
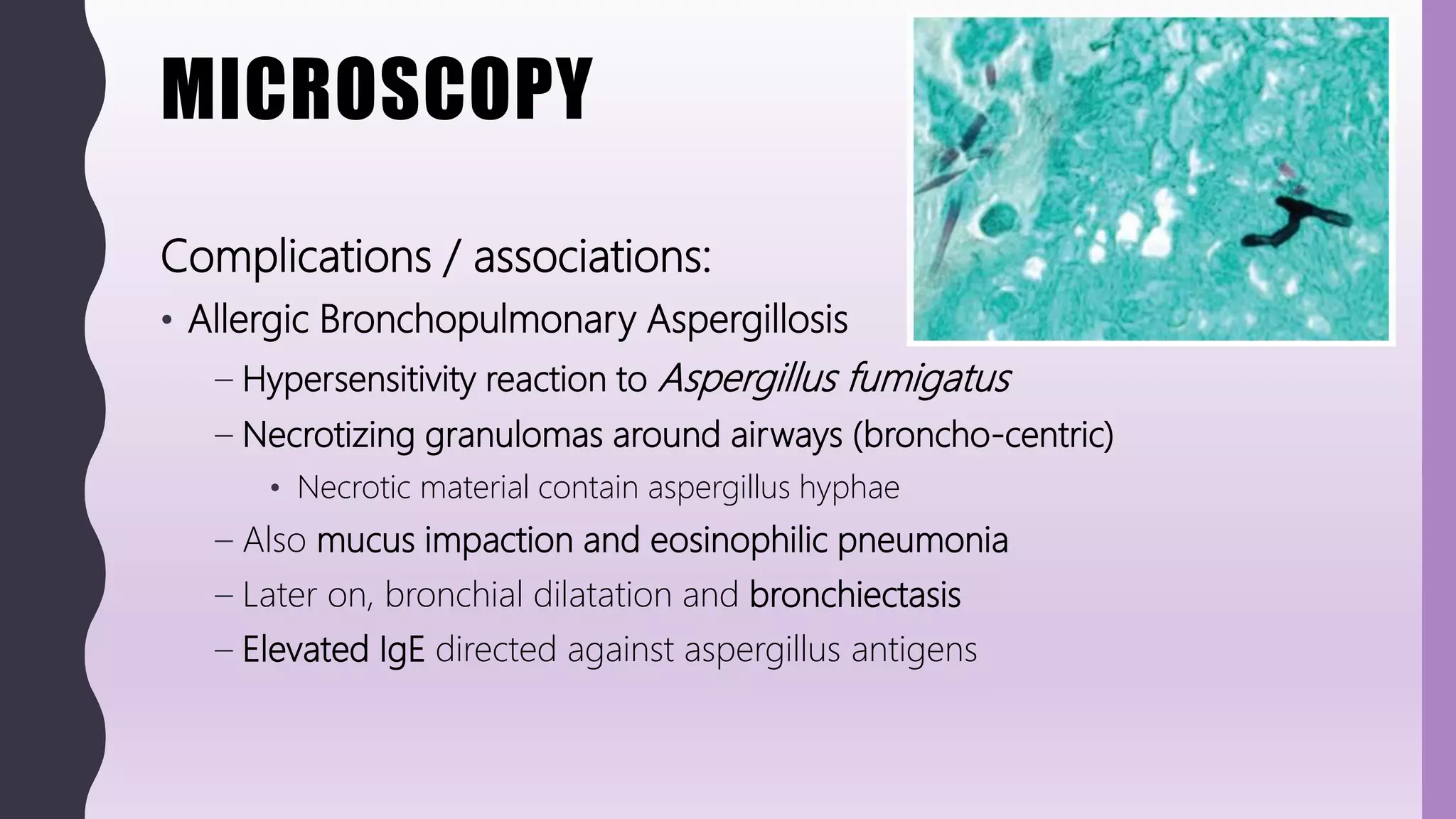
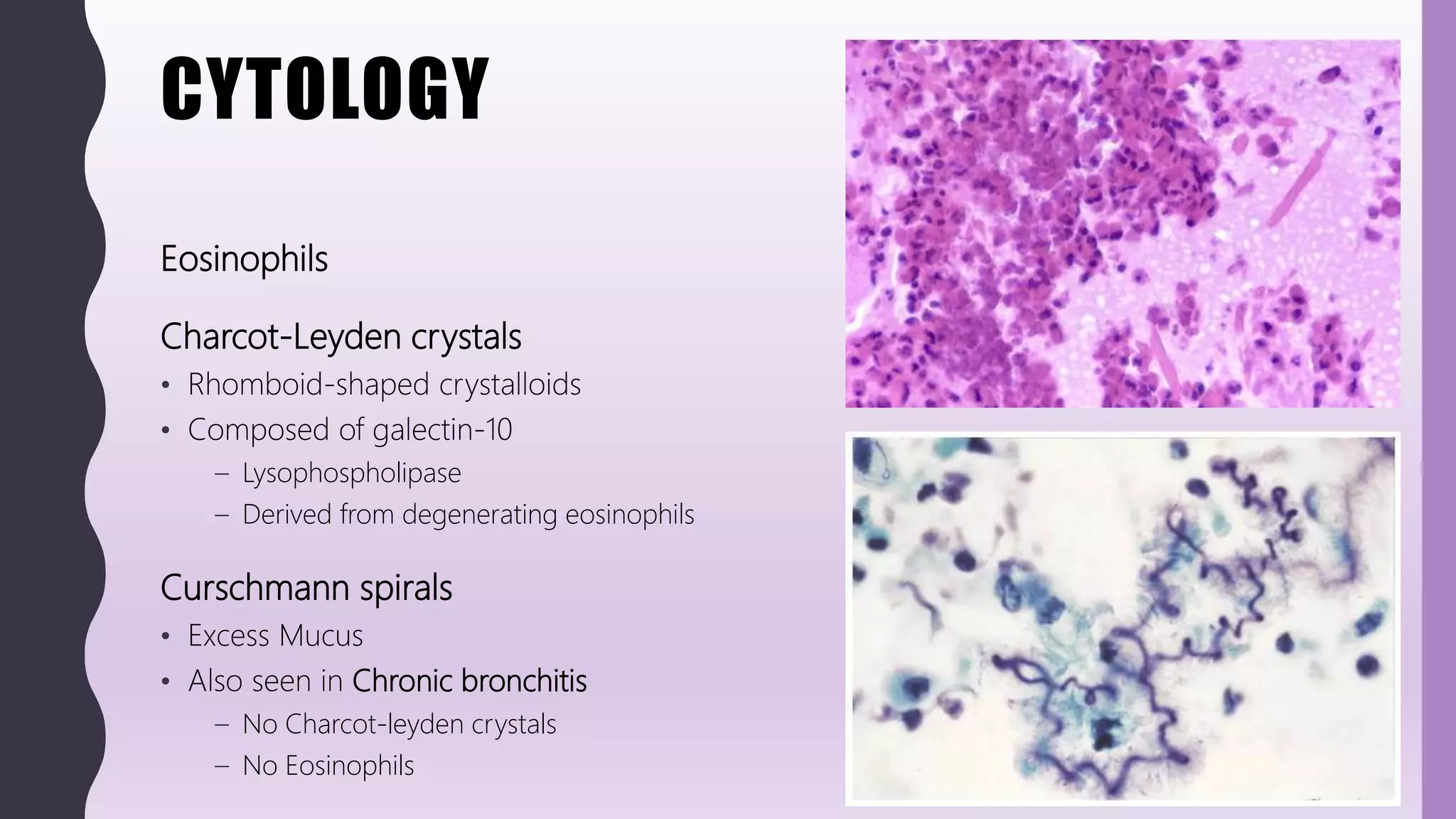
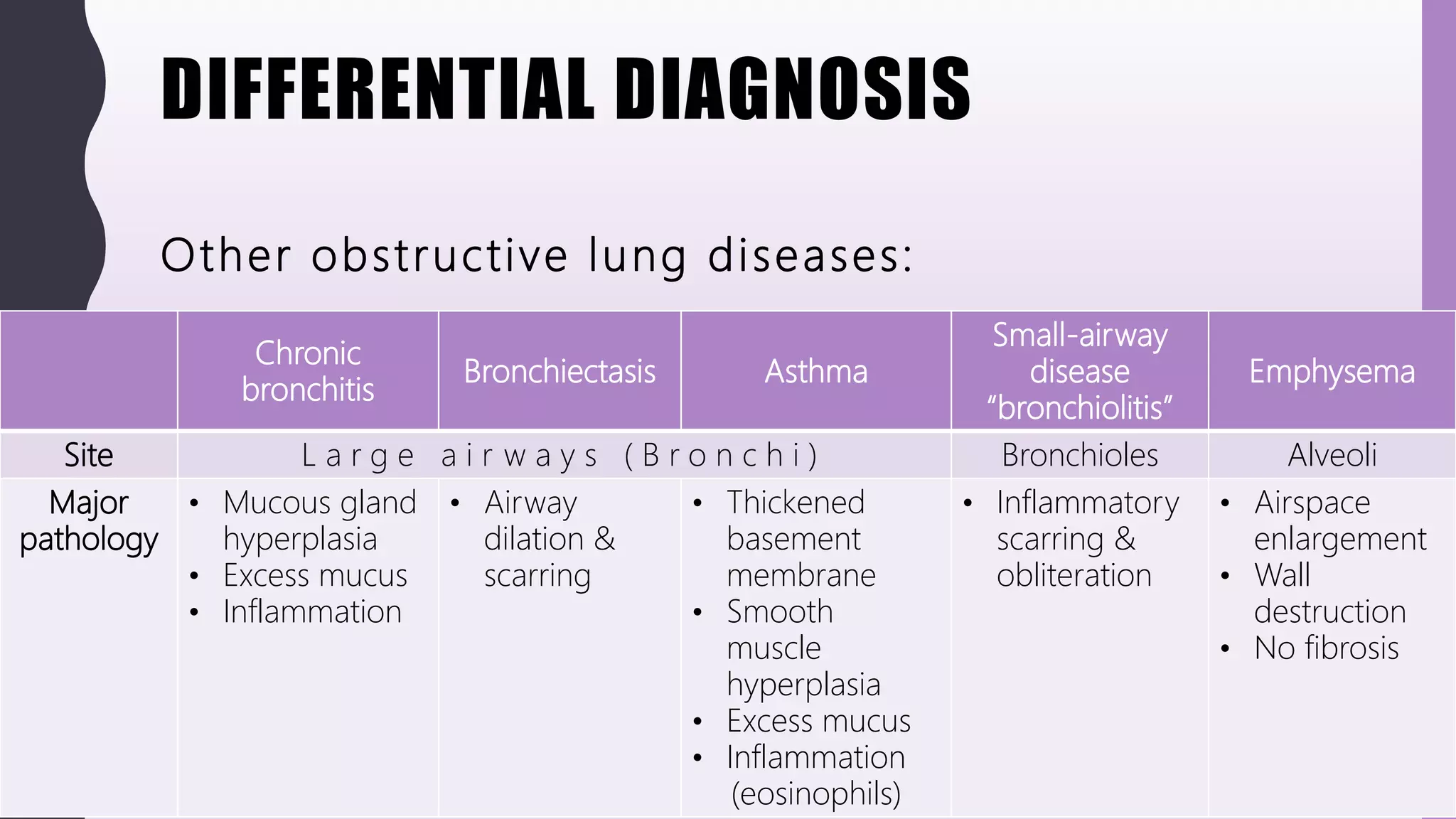
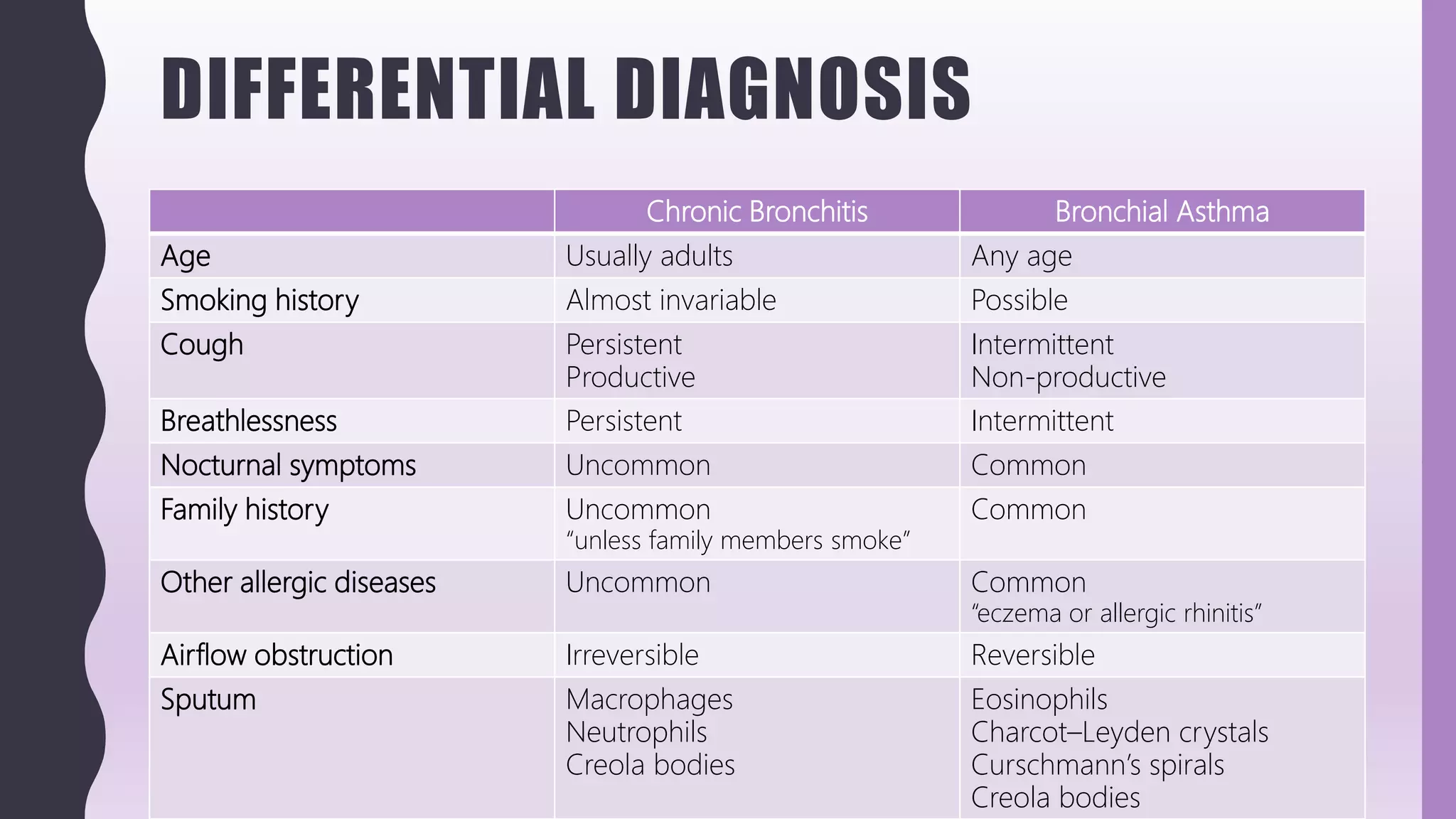
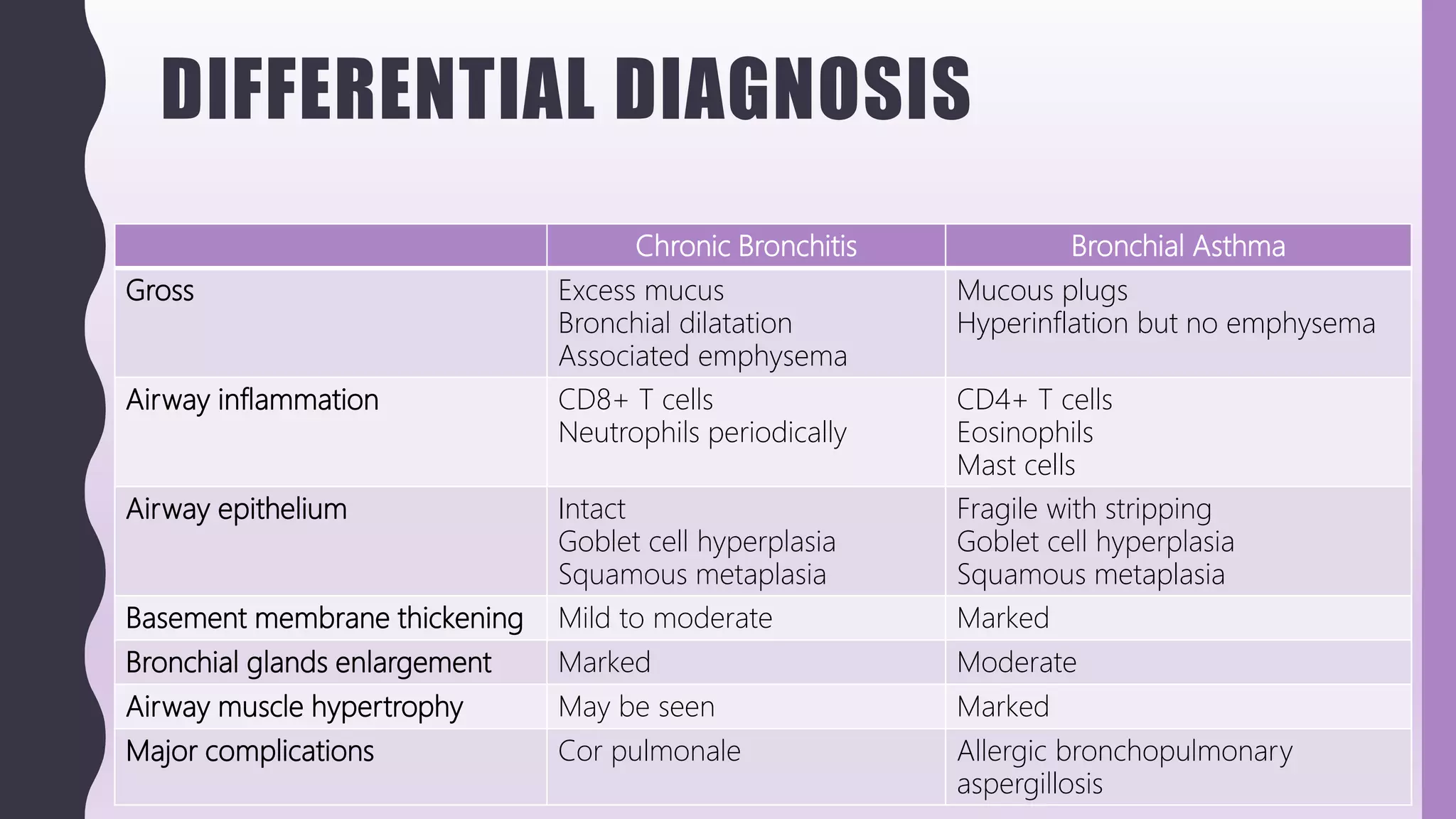
The document discusses asthma, including that it is a chronic inflammatory disorder of the airways causing widespread but reversible airflow obstruction. It describes the pathogenesis of asthma including the role of type 1 hypersensitivity reactions and inflammatory cells like eosinophils. Differential diagnoses are provided and treatment involves avoiding triggers and using bronchodilators, corticosteroids, and other drugs.