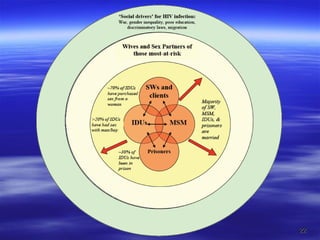
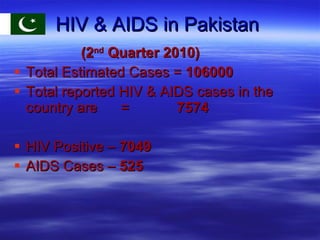
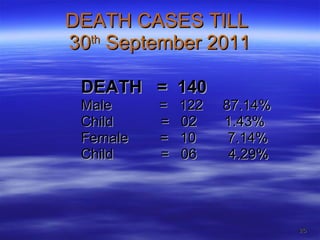
The document provides information about HIV/AIDS in Pakistan, including:
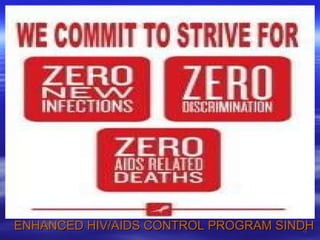
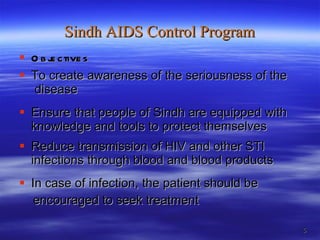
1) It discusses the objectives and infrastructure of the Enhanced Sindh AIDS Control Program, including voluntary counseling and testing centers, STI clinics, and PPTCT centers.
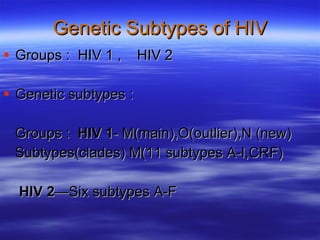
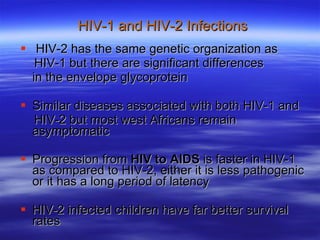
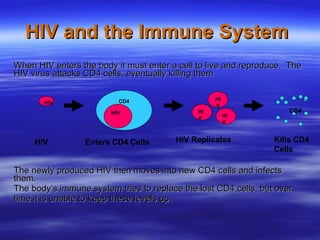
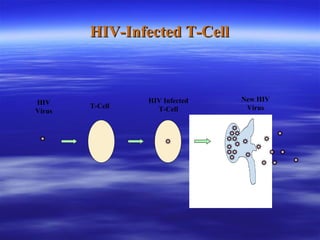
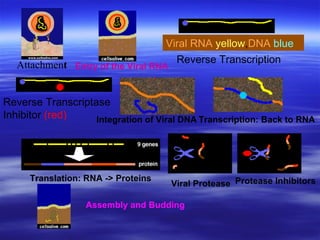
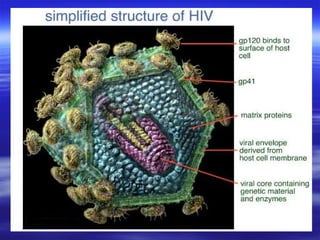
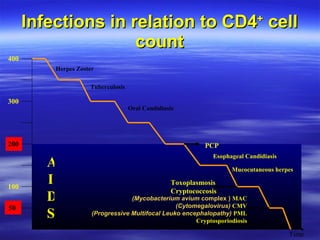
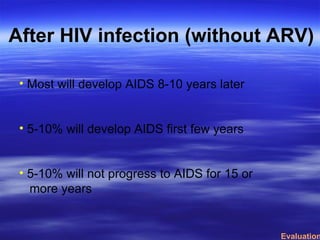
2) It provides a brief history of HIV, noting it originated from chimpanzees and was first identified in the US in 1981. HIV attacks and destroys CD4 cells, eventually causing AIDS.
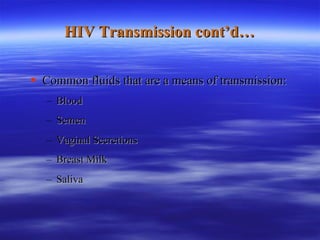
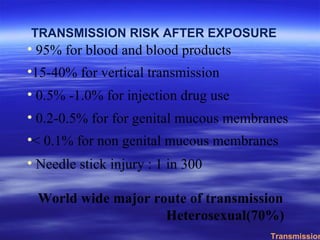
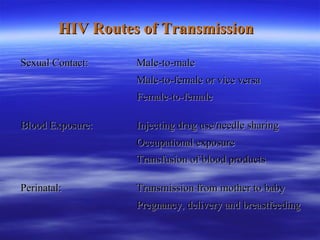
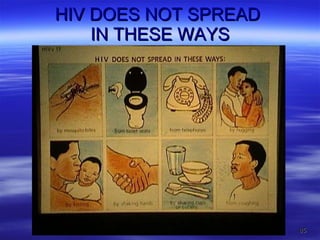
3) It discusses HIV transmission, noting the major routes are sexual contact, exposure to infected blood or blood products, and from mother to child during pregnancy, birth, or breastfeeding.



![African Simean [Green] Chimpanzee](https://image.slidesharecdn.com/animationshivaidsdrmunawar3-13252427658846-phpapp01-111230050046-phpapp01/85/HIV-AIDS-Dr-Munawar-Khan-9-320.jpg)