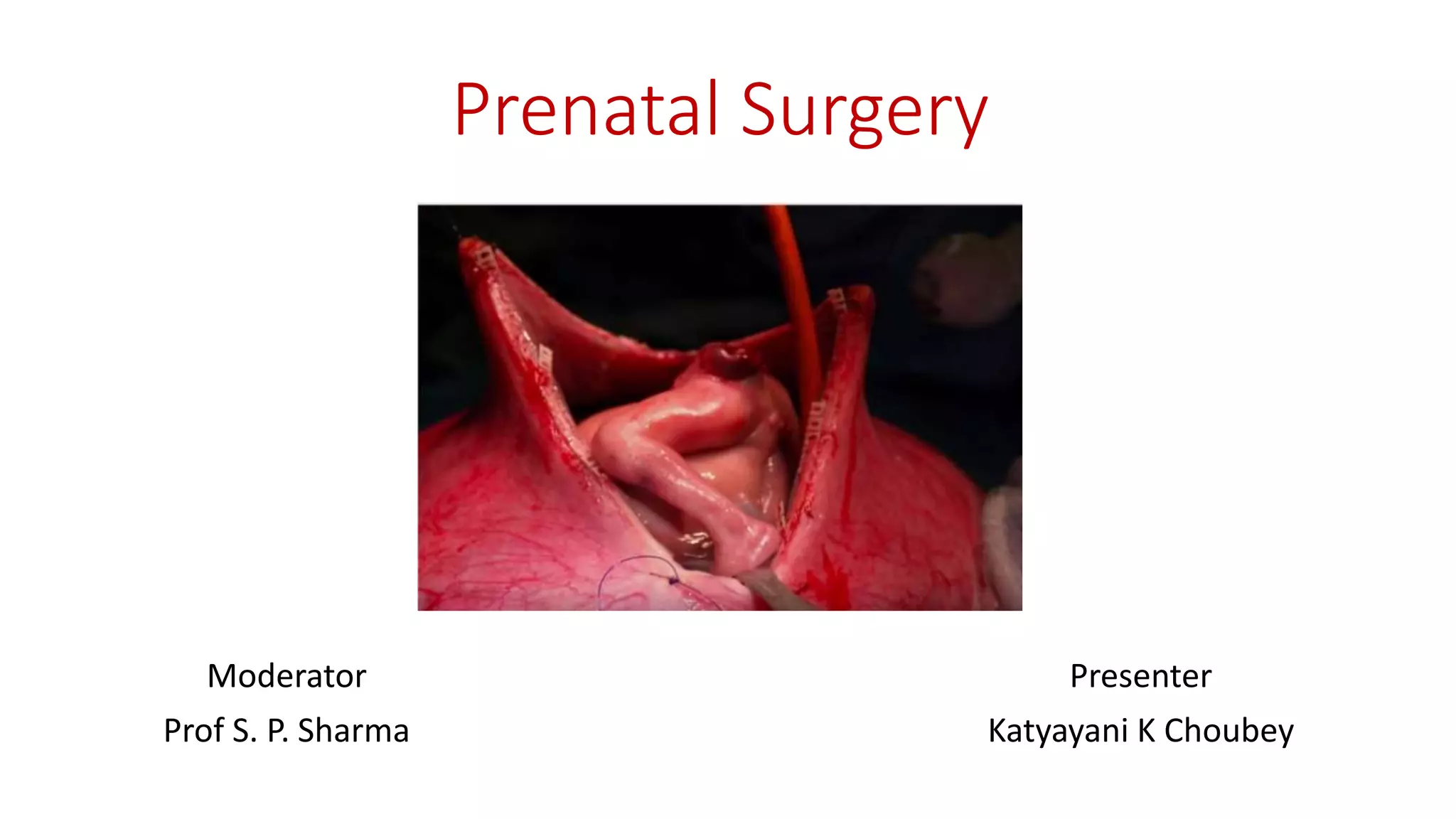
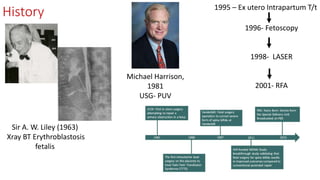
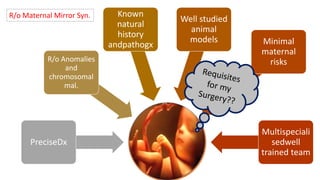
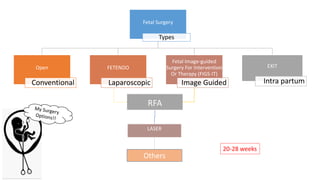
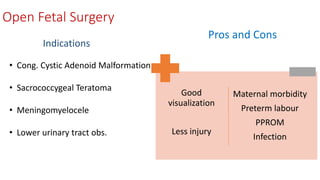
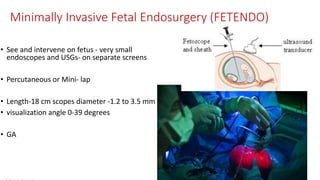
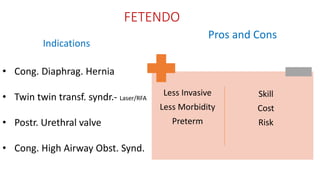
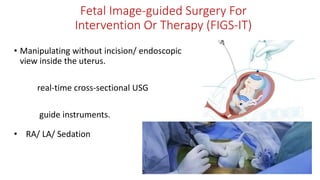
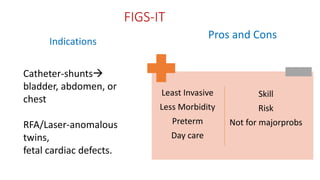
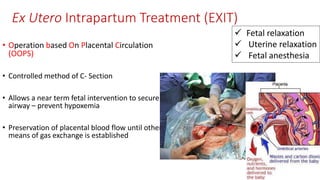
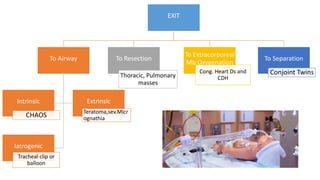
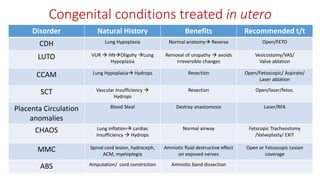
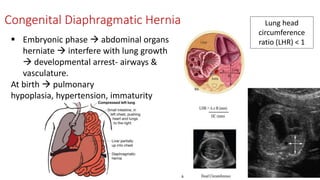
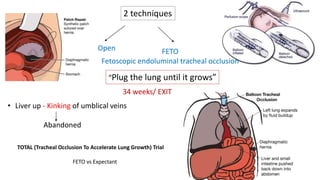
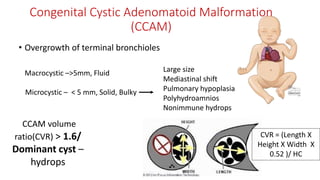
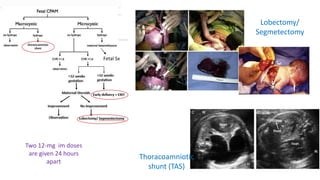
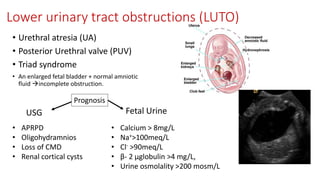
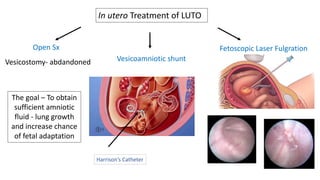
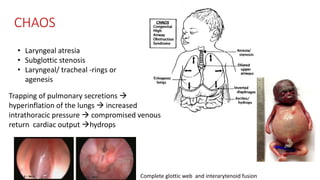
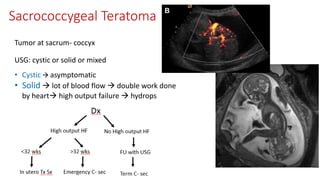
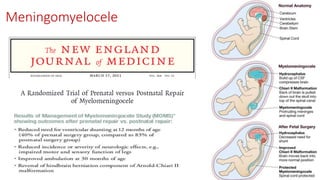
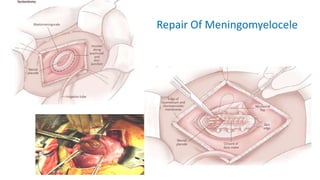
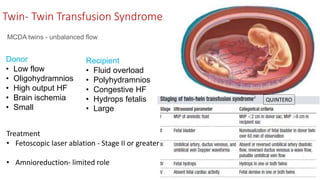
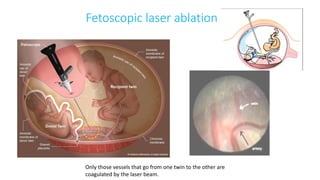
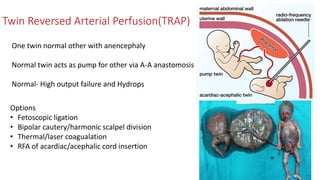
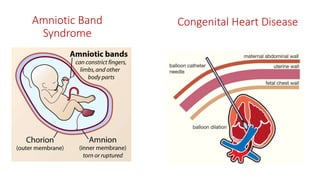
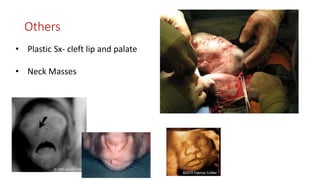
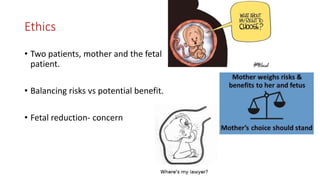
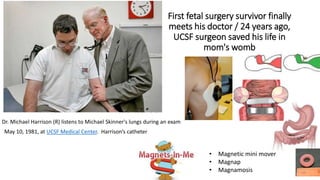
Prenatal surgery, also known as fetal surgery, involves performing surgery on a fetus while still in the womb. It can treat certain birth defects to prevent or lessen health issues. Fetal surgery has advanced from open fetal procedures to minimally invasive techniques using fetoscopy or fetal image-guided interventions. Conditions commonly treated include congenital diaphragmatic hernia, lower urinary tract obstructions, cystic adenomatoid malformation, and twin-twin transfusion syndrome. Fetal surgery requires a multidisciplinary team and careful patient selection due to risks of preterm birth and other maternal-fetal complications. Outcomes are continually improving as the field further develops new techniques and treatments.