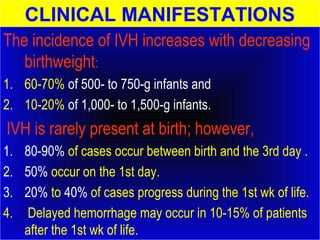
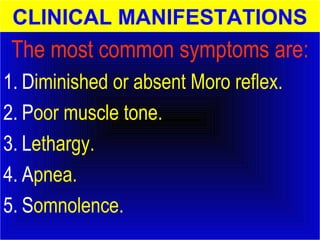
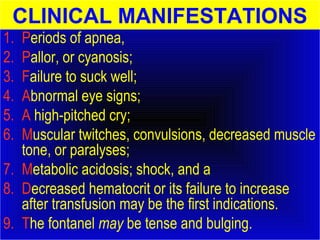
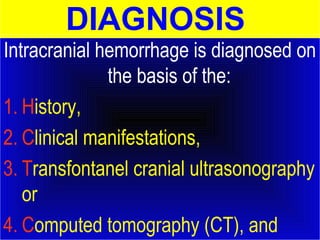
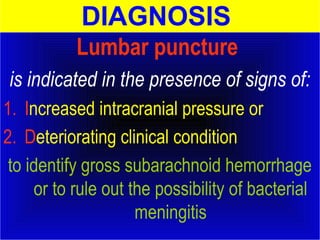
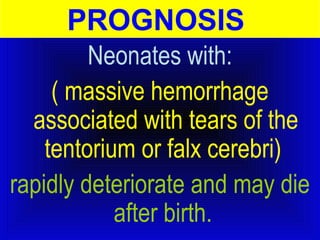
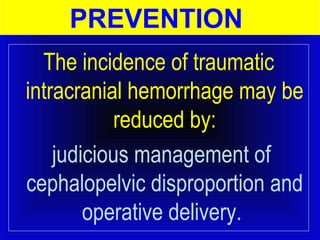
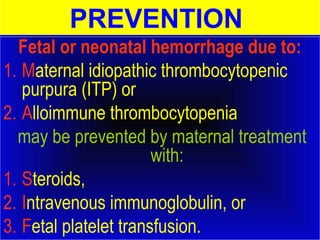
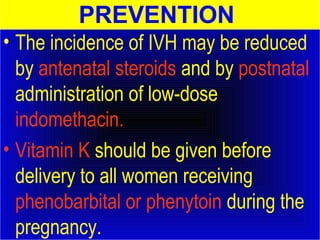
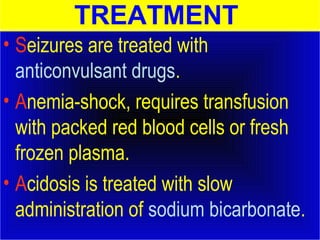
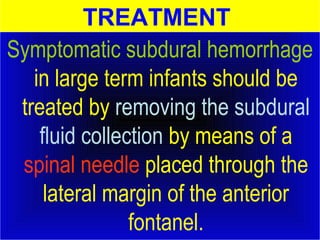
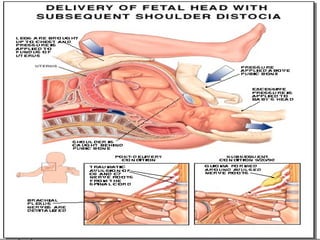
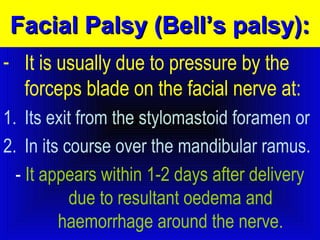
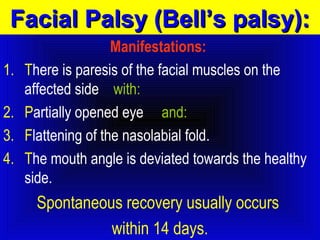
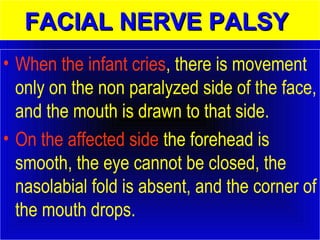
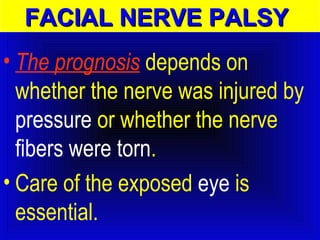
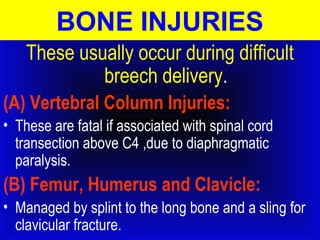
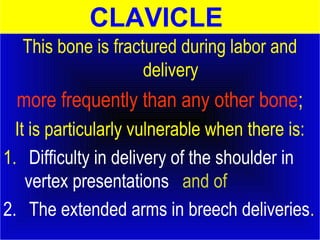
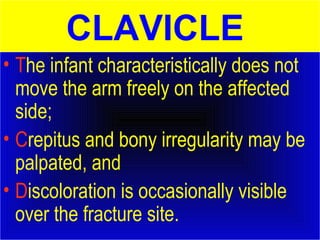
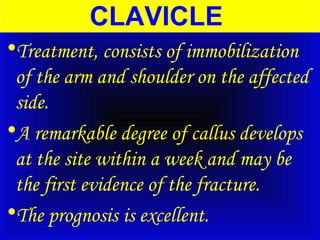
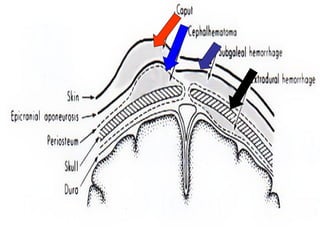
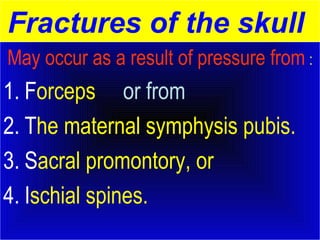
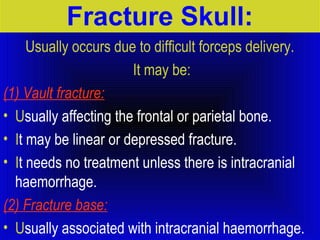
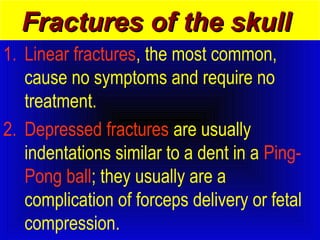
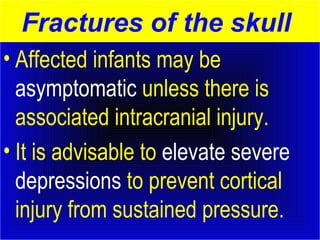
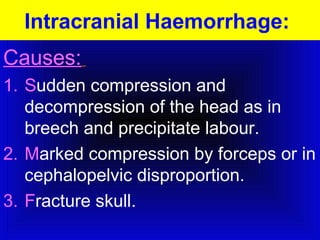
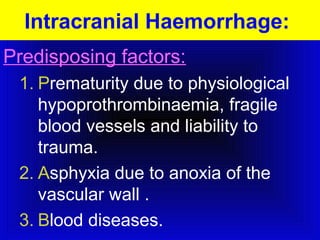
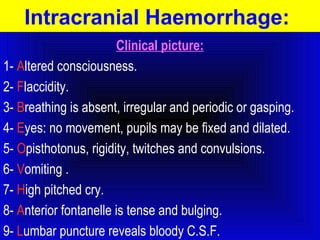
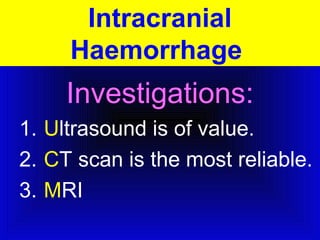
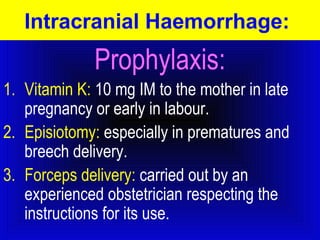
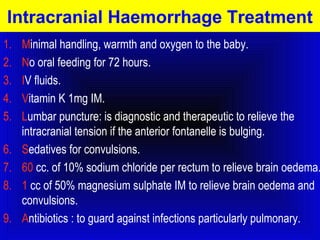
Fetal birth injuries can be avoidable or unavoidable, occurring during labor and delivery. They may result from inappropriate medical care or despite skilled care. Common injuries include skull fractures, cephalohematomas, and intracranial hemorrhages. Intracranial hemorrhages can occur from birth trauma, asphyxia, or vascular issues and often involve the ventricles in premature infants. Symptoms may include apnea, lethargy, and bulging fontanel. Diagnosis is via ultrasound, CT scan, or lumbar puncture. Treatment focuses on stabilization, antibiotics if needed, and managing increased intracranial pressure. Prevention strategies include judicious delivery management and antenatal steroids for premature





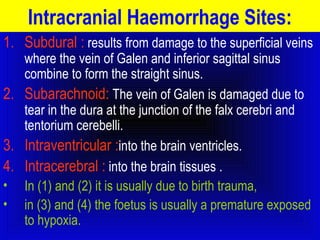
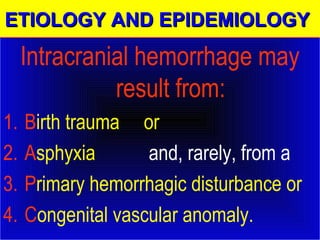
![ETIOLOGY AND EPIDEMIOLOGY
• Intracranial hemorrhages often
involve the ventricles
( intraventricular hemorrhage [IVH])
of premature infants delivered
spontaneously without apparent
trauma.](https://image.slidesharecdn.com/fetal-birth-injuries1-121204143707-phpapp02-141106130558-conversion-gate02/85/Fetal-birth-injuries-36-320.jpg)