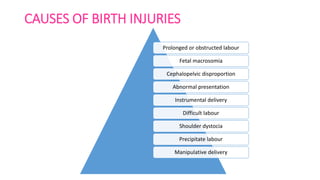
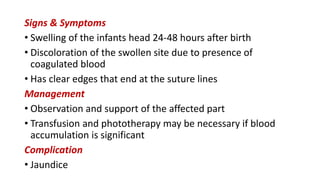
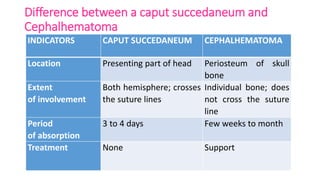
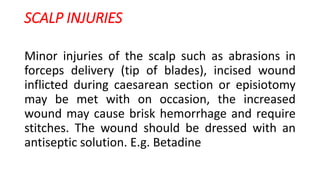
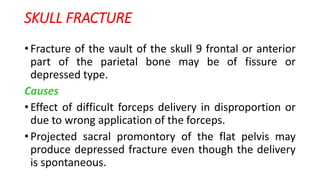
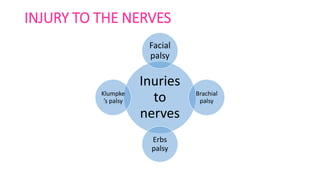
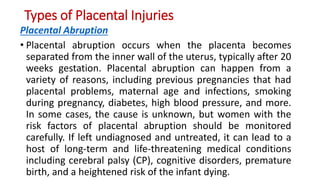
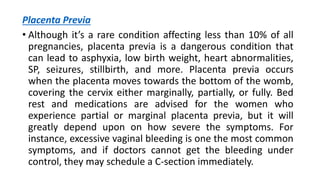
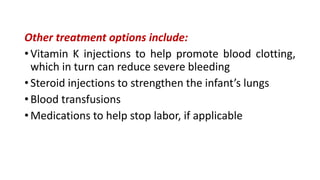
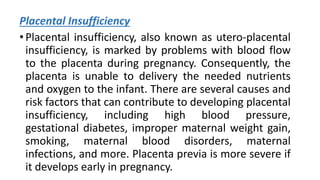
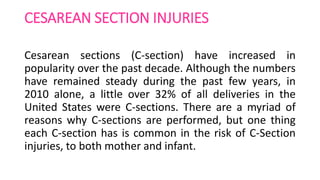
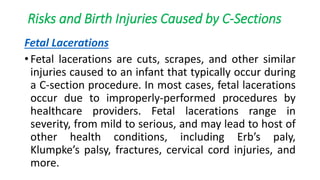
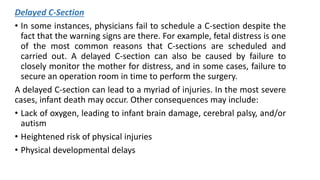
The document discusses the various types of birth injuries that can occur during labor and delivery, including classifications such as soft tissue injuries, cranial nerve injuries, and fractures. It outlines high-risk factors, causes, clinical features, prevention strategies, and treatment options for these injuries, emphasizing the importance of monitoring and proper management. Additionally, it covers specific conditions like intracranial hemorrhage and persistent pulmonary hypertension in newborns, and how timely interventions can mitigate complications.