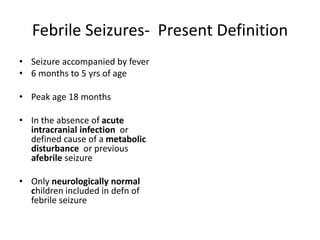
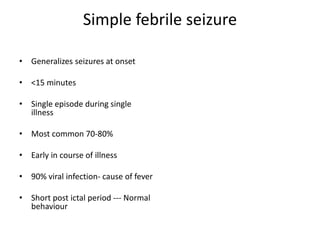
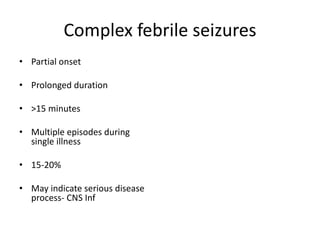
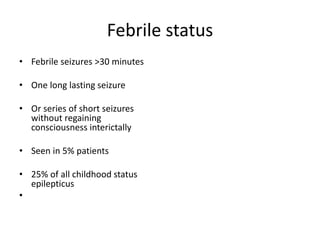
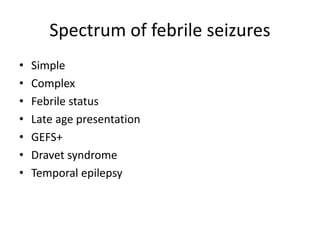
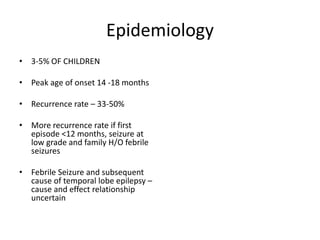
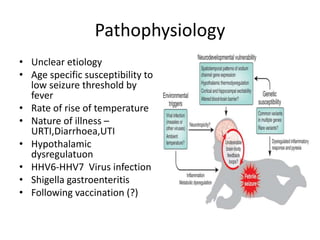
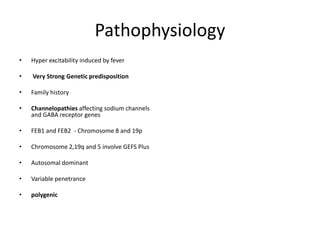
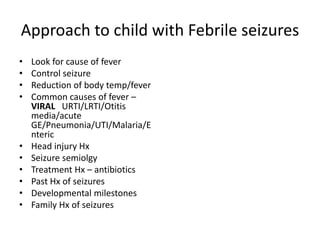
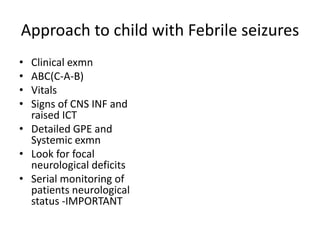
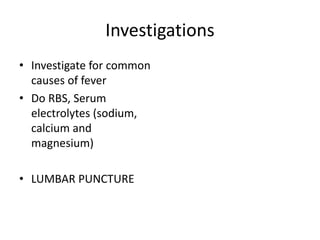
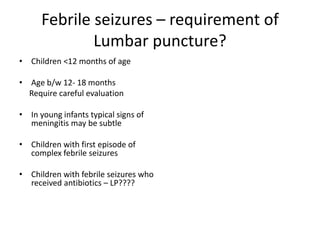
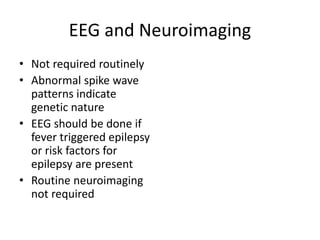
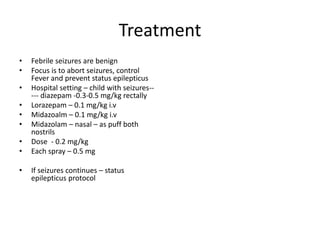
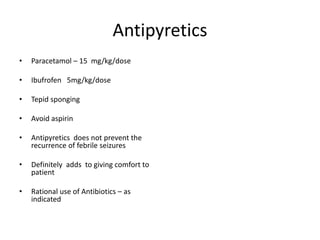
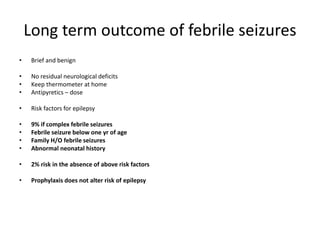
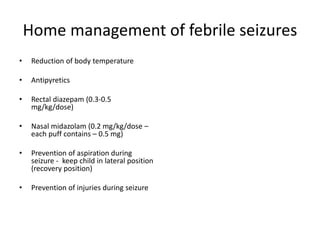
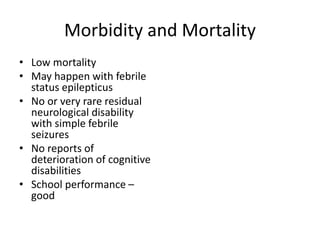
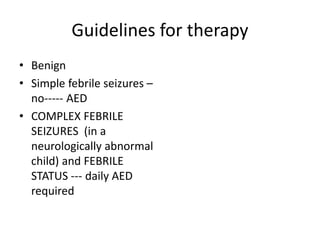
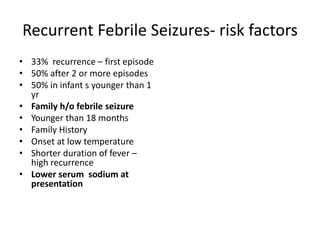
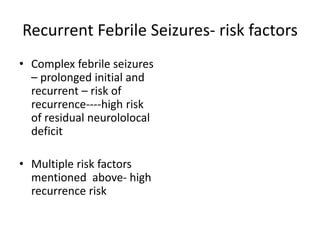
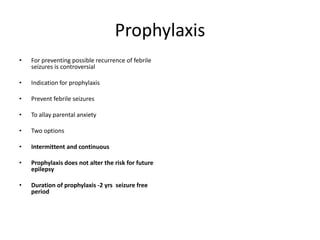
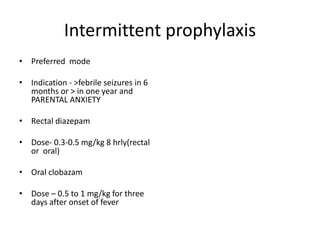
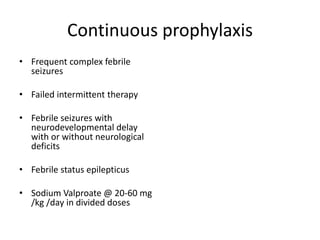
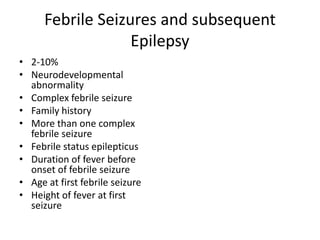
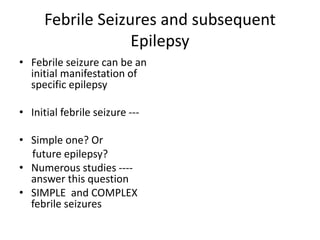
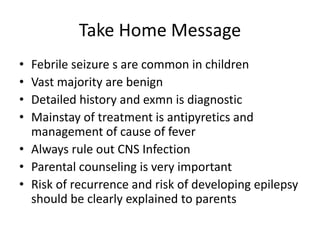
Febrile seizures are the most common type of seizure seen in children under 5 years old. While they can be alarming for parents, the majority are benign and have an excellent prognosis. Febrile seizures are classified as simple or complex based on features like duration, recurrence, and onset. Investigations are usually not needed but may include lumbar puncture in young infants to rule out infection. Treatment focuses on controlling fever and preventing prolonged seizures. Parents should be reassured that febrile seizures rarely cause neurological issues and most children outgrow them. Recurrence risks are highest for those under 18 months, with family history or complex initial seizures. Prophylaxis may be used to prevent recurrence but does not impact later epilepsy risk.