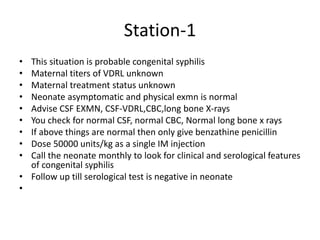
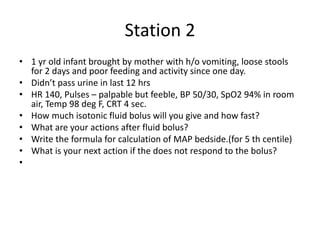
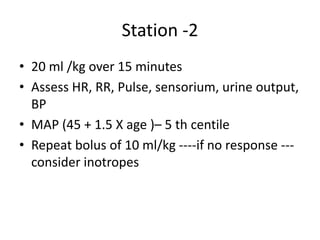
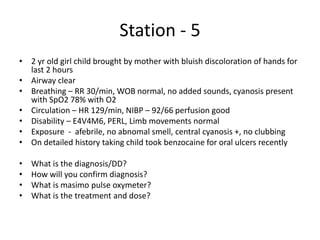
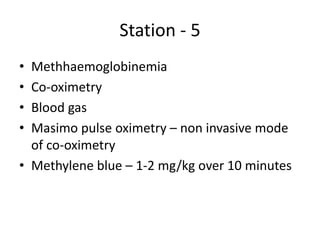
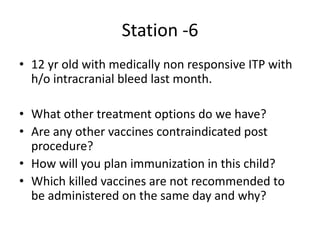
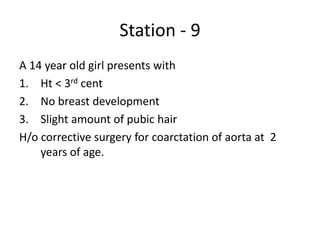
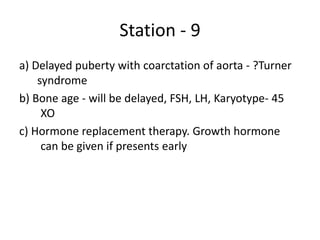
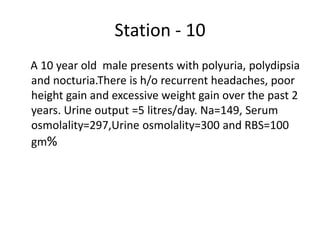
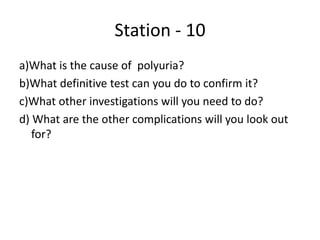
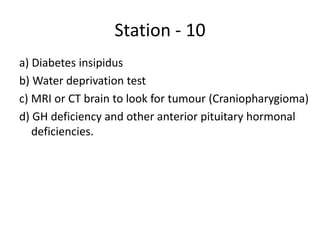
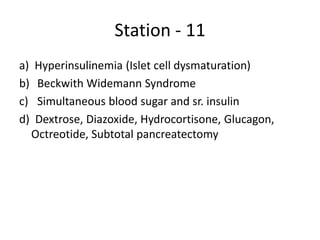
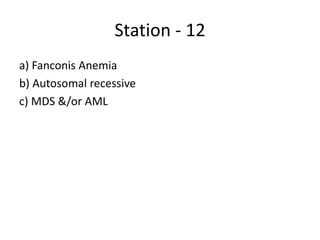
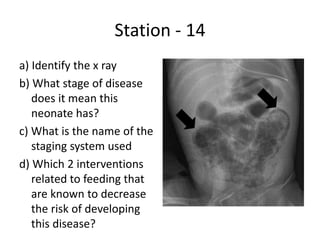
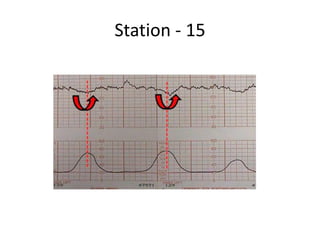
This document contains summaries of 16 patient case scenarios presented at an OSCE exam. For each case, the key presenting signs and symptoms, likely diagnosis, relevant diagnostic tests and treatment recommendations are outlined in 1-3 concise sentences. The cases cover a range of pediatric topics including neonatal jaundice, dehydration, rashes, developmental delays, diabetes insipidus, and more.