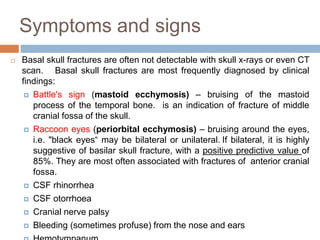
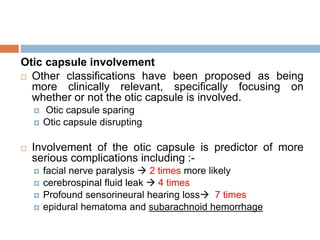
The document discusses facial nerve disorders and paralysis, detailing both central and peripheral causes, with central causes including brain abscesses and strokes, while peripheral causes primarily involve idiopathic lesions and infections. It highlights acoustic neuroma as a common tumor affecting the facial nerve, outlines diagnostic methods, and treatment options like surgery and corticosteroids. Additionally, the document covers conditions such as Bell's palsy and Ramsay Hunt syndrome, including their clinical features, diagnosis, and management strategies.