This document discusses facial nerve paralysis, including:
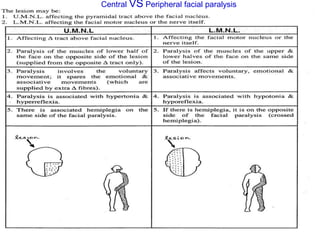
- The anatomy of the facial nerve and branches that innervate facial muscles.
- Common causes of facial nerve paralysis like Bell's palsy.
- Evaluating facial nerve paralysis through examining facial muscles, taste sensation, lacrimation, and nerve conduction velocity.
- Treating facial nerve paralysis with physical therapy including heat, electrotherapy, exercises and occasionally splinting.