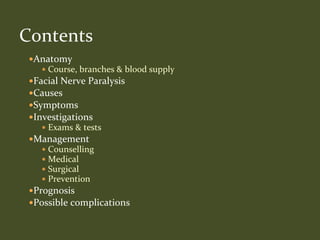
The document discusses facial nerve paralysis, including:
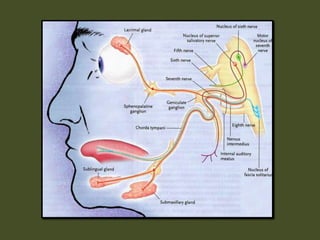
- The facial nerve controls facial muscles and taste, emerging from the brainstem.
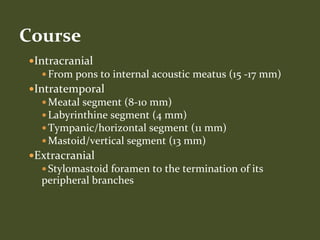
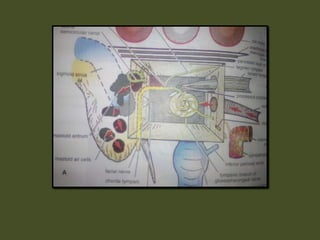
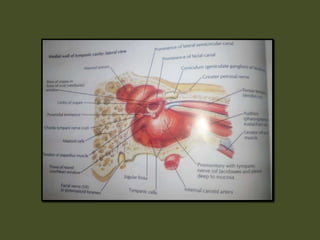
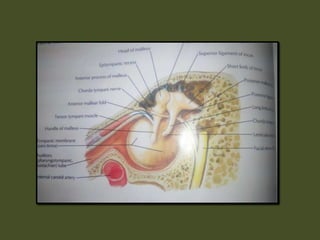
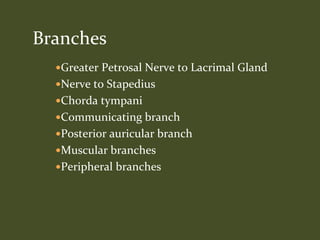
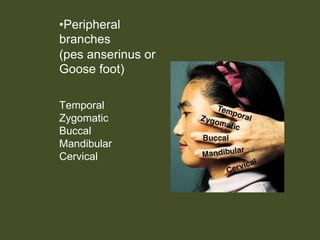
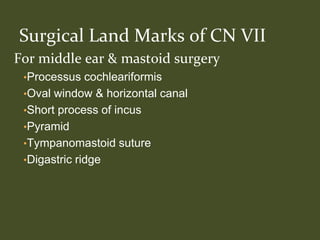
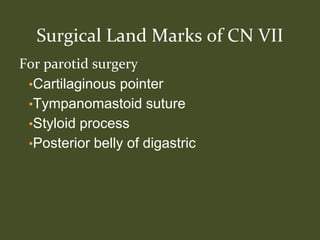
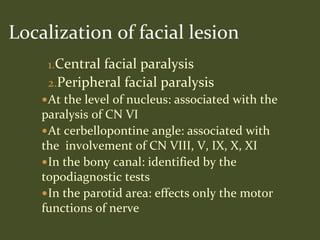
- It describes the anatomy and course of the facial nerve from the brainstem to its branches.
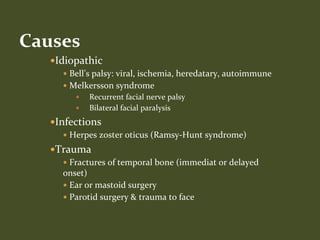
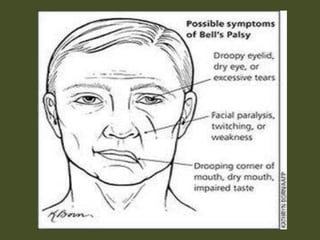
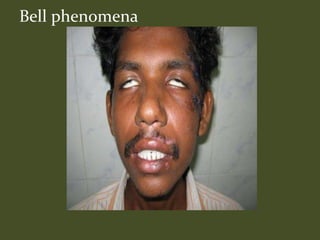
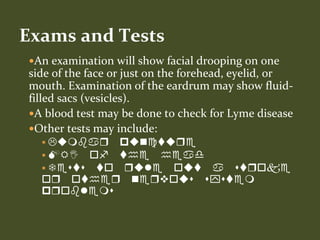
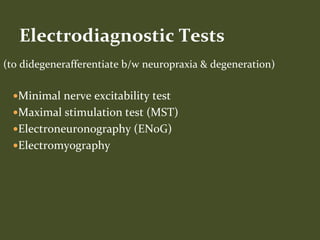
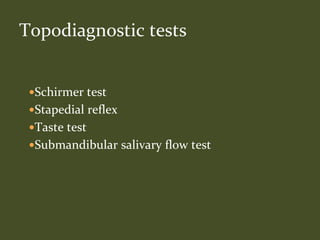
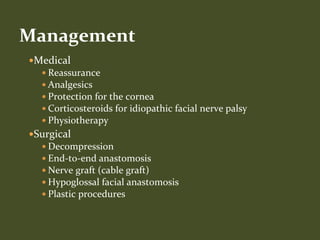
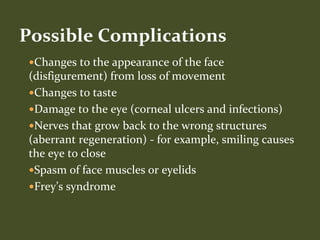
- Causes of facial nerve paralysis include Bell's palsy, infections, trauma, tumors, and other systemic diseases. Symptoms include facial drooping and difficulties with facial expressions. Exams and tests help diagnose the cause and location of damage. Management includes medical and sometimes surgical approaches, with varying prognosis and potential complications.