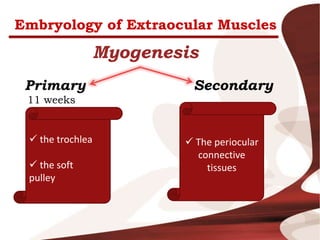
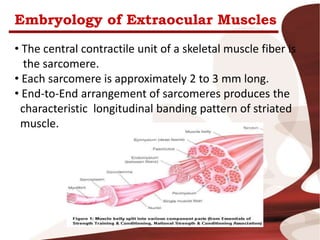
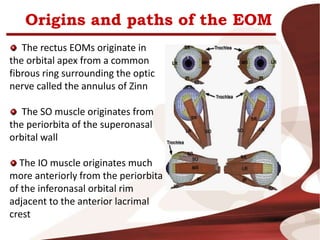
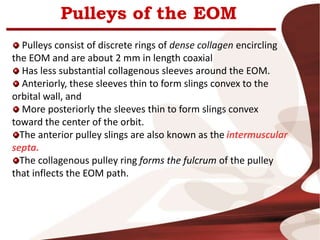
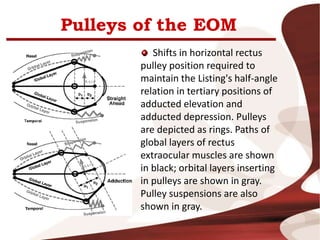
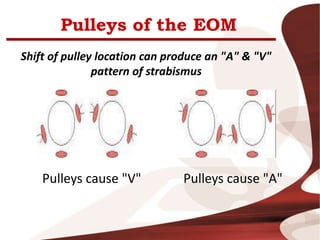
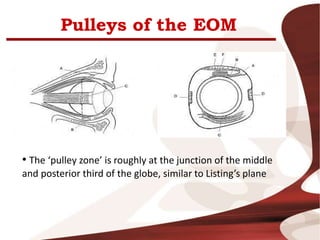
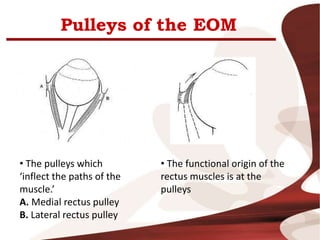
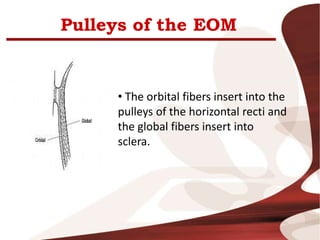
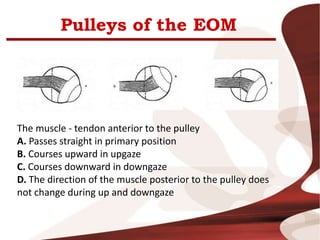
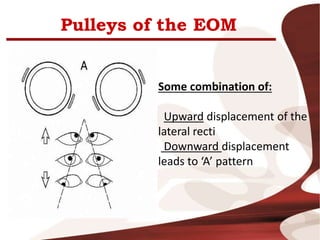
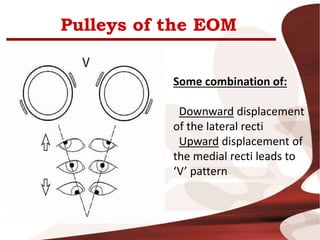
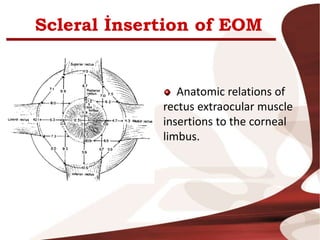
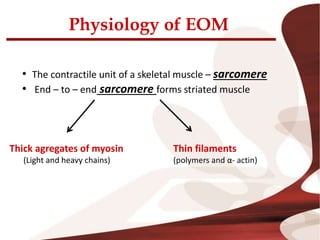
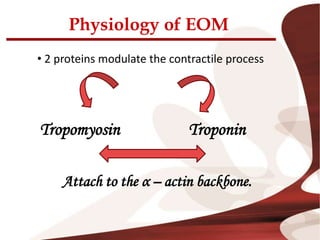
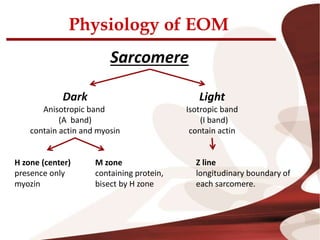
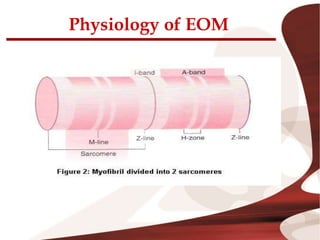
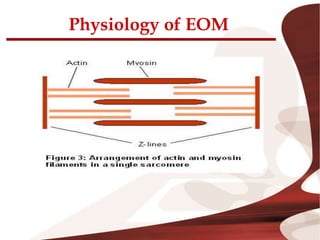
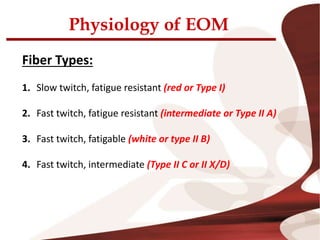
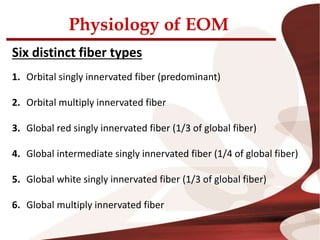
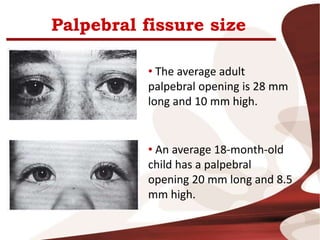
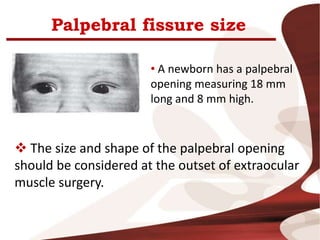
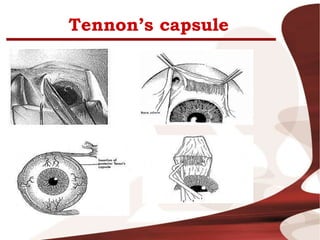
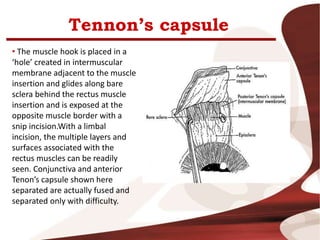
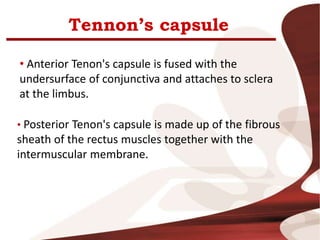
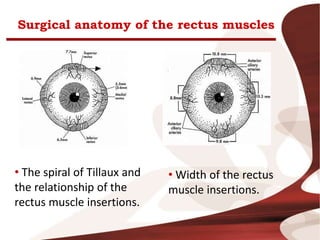
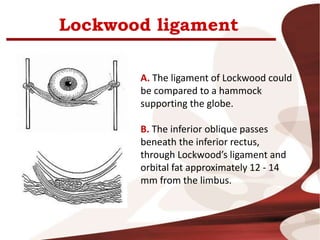
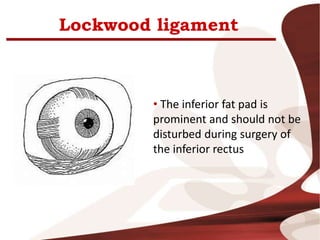
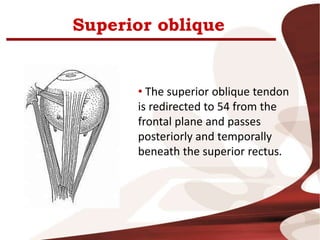
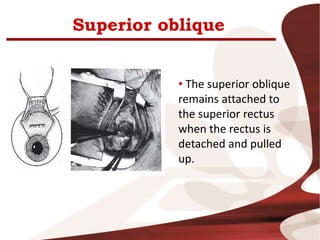
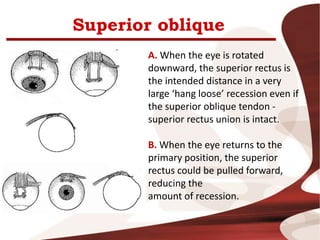
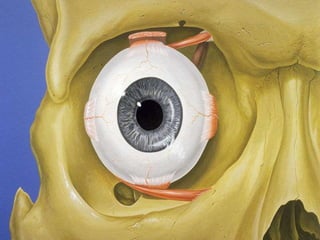
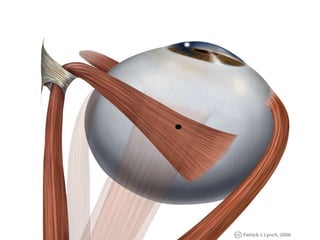
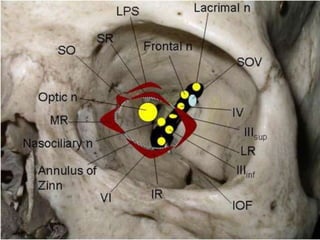
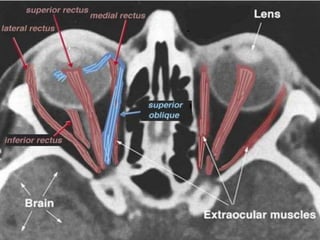
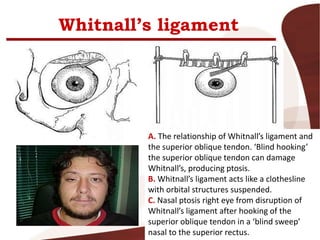
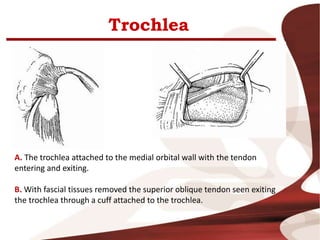
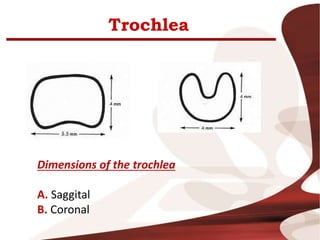
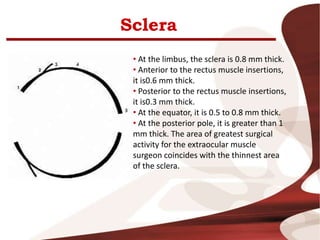
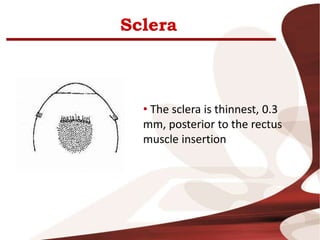
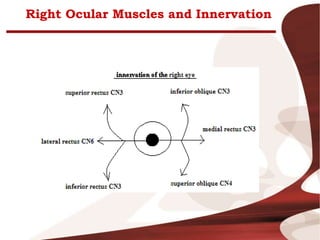
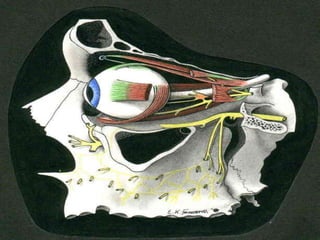
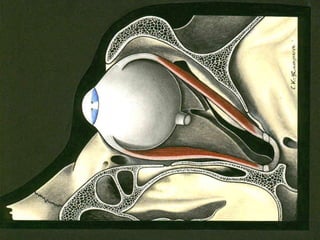
The document discusses the anatomy and embryology of the extraocular muscles. It covers topics such as the origin of the muscles from mesoderm and neural crest, the development of pulleys and connective tissues, the internal structure of the muscles including fiber types, and the surgical anatomy of structures like the rectus muscles and Tenon's capsule. The physiology of muscle contraction and the characteristics that make extraocular muscles unique are also summarized.