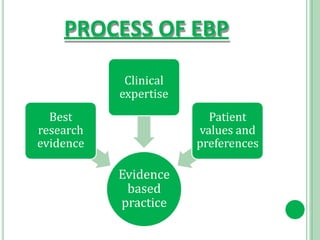
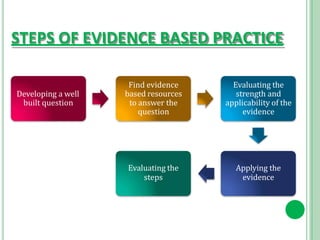
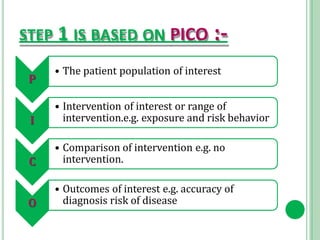
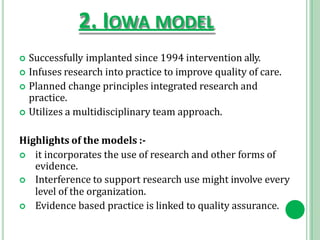
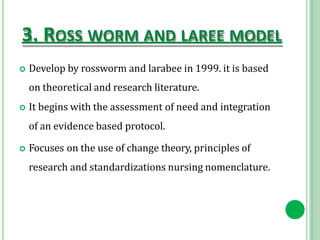
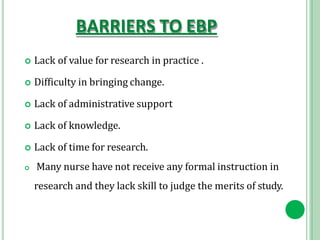
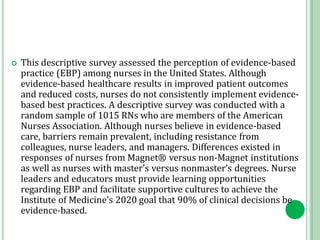
This document discusses evidence-based practice (EBP) in nursing. It defines EBP as making clinical decisions based on the best available research evidence, clinical expertise, and patient values. The document outlines the steps of EBP, which include developing a focused question, finding evidence, evaluating the evidence, applying it, and evaluating outcomes. It discusses models for EBP implementation, including the Stetler, Iowa, and Rosswurm and Larrabee models. Barriers to EBP include lack of time, skills and support, while benefits include improved patient outcomes. Nurse leaders play a key role in facilitating EBP through training, resources and supportive cultures.