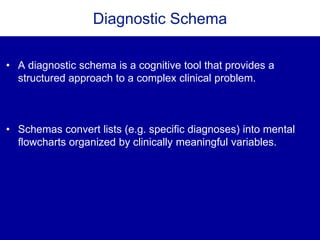
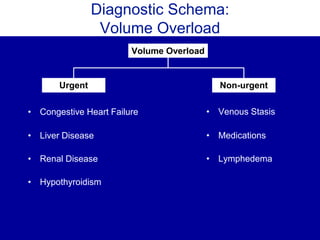
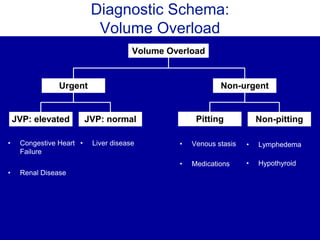
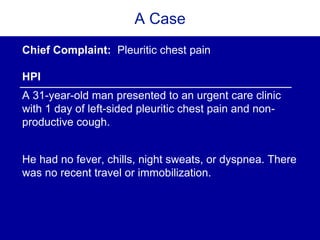
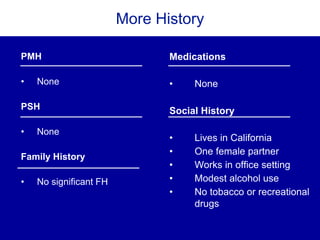
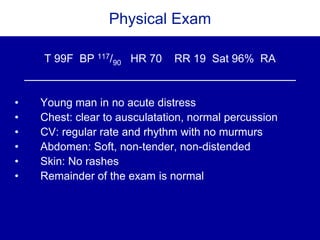
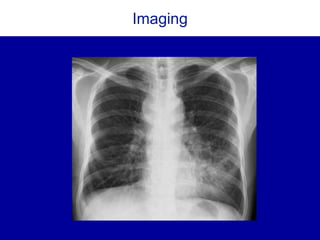
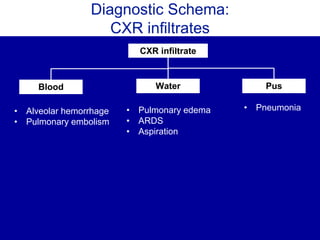
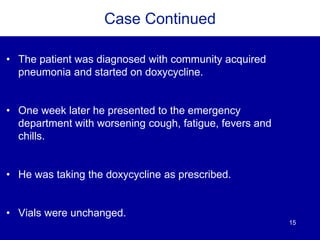
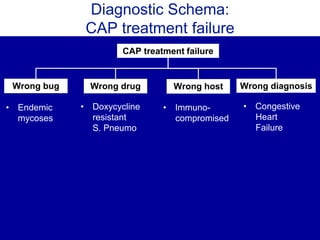
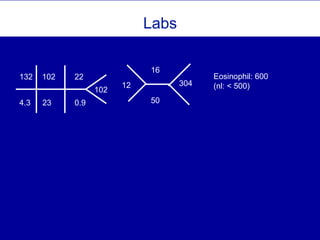
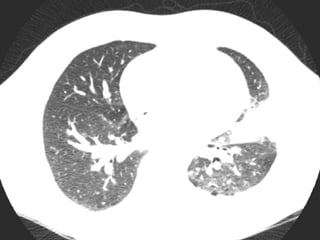
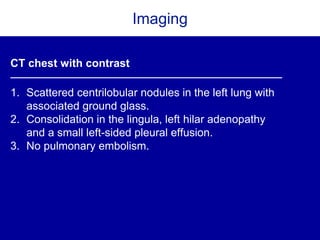
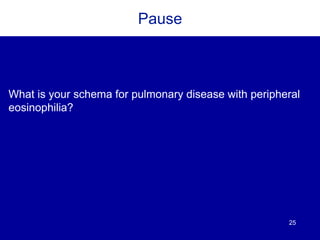
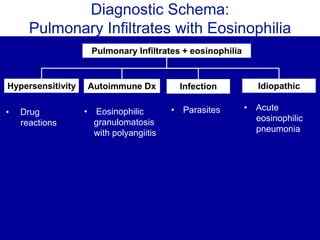
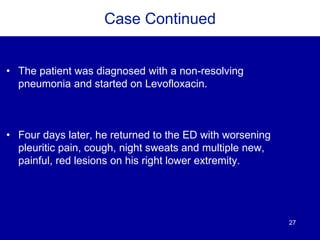
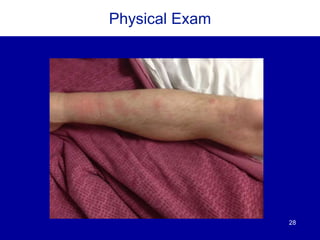
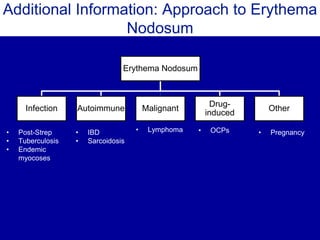
The document discusses the use of diagnostic schemas as cognitive tools for structured clinical reasoning, particularly in addressing complex medical cases like pleuritic chest pain and community-acquired pneumonia. It outlines a case study involving a patient diagnosed with coccidioidomycosis after presenting with pneumonia symptoms, providing insights on differential diagnosis and treatment. Additionally, it emphasizes the importance of travel history in diagnosis and the role of schema in managing clinical decision-making.