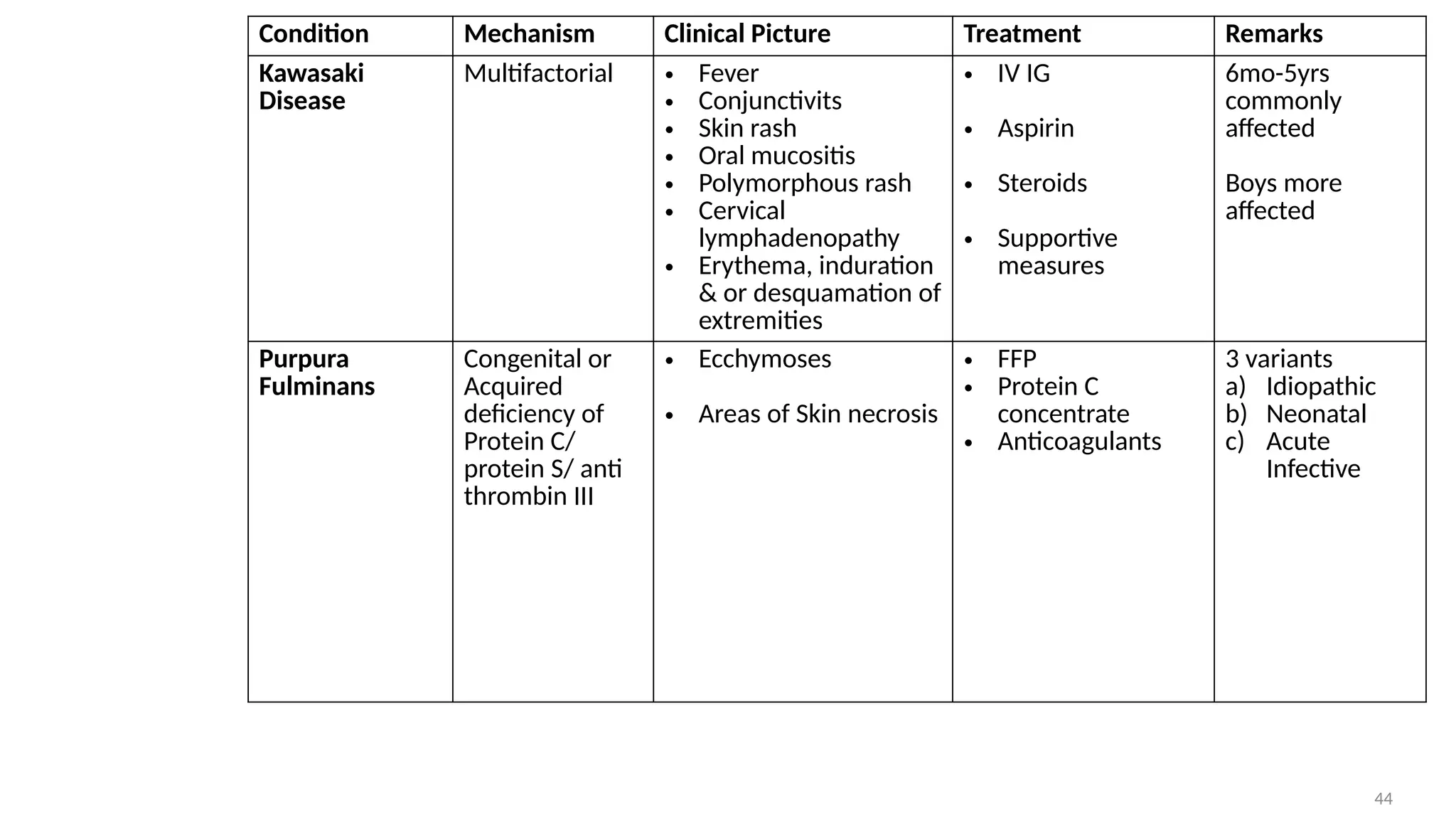
The document outlines various dermatological emergencies that can be life-threatening if not promptly diagnosed and treated. Key conditions discussed include erythroderma, severe drug reactions, and infections, each requiring multifaceted management approaches in emergency settings. It emphasizes the critical role of early recognition and intervention to improve patient outcomes.