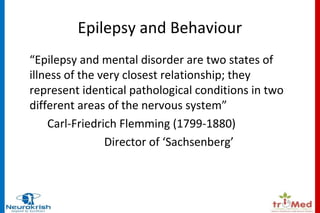
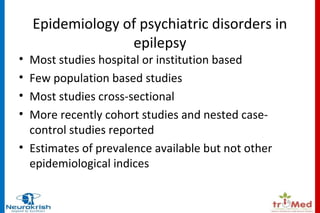
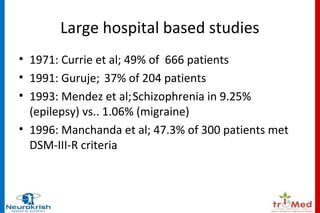
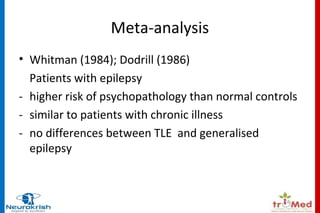
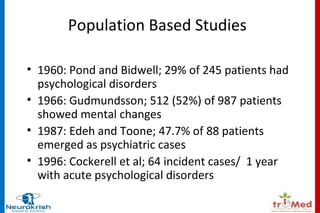
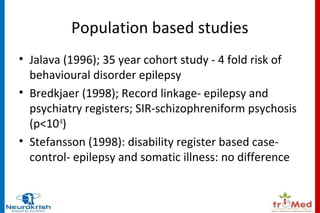
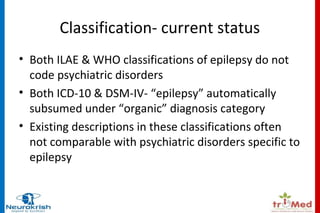
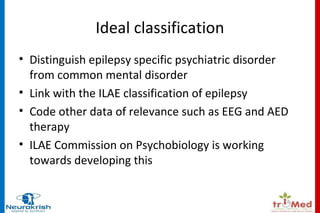
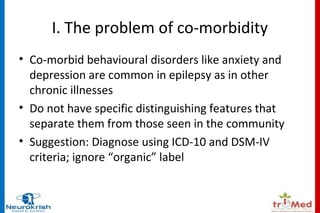
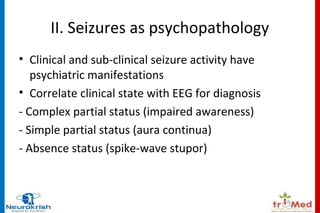
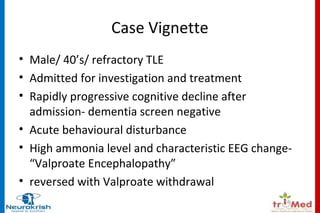
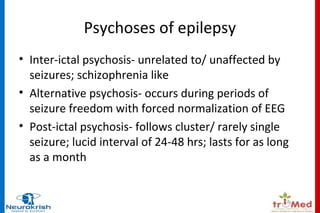
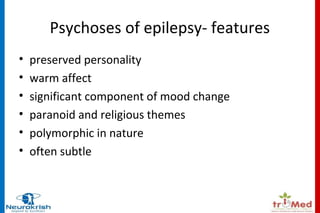
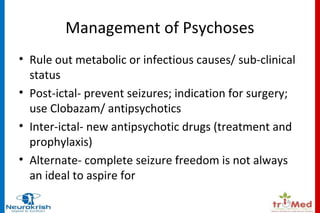
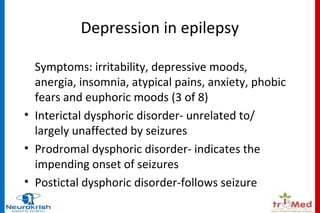
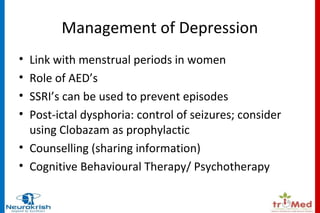
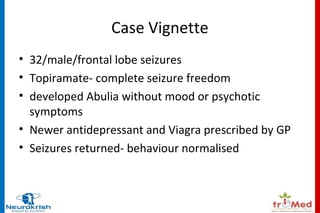
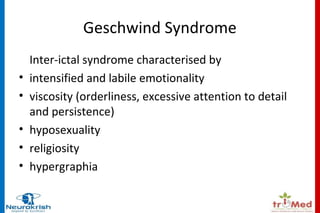
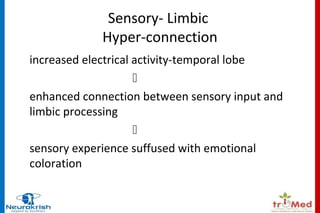
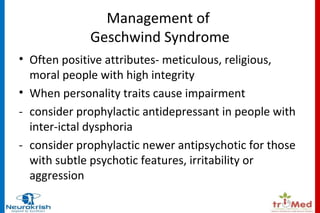
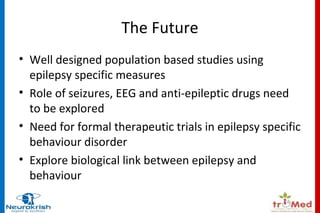
The document provides an overview of the relationship between epilepsy and behavioral disorders, highlighting the prevalence of psychiatric issues in patients with epilepsy. It discusses the challenges in classifying these disorders, the impact of anti-epileptic drugs, and the different types of psychoses associated with epilepsy. Furthermore, it emphasizes the need for better population-based studies and the consideration of personalized treatment approaches for managing co-morbid conditions.