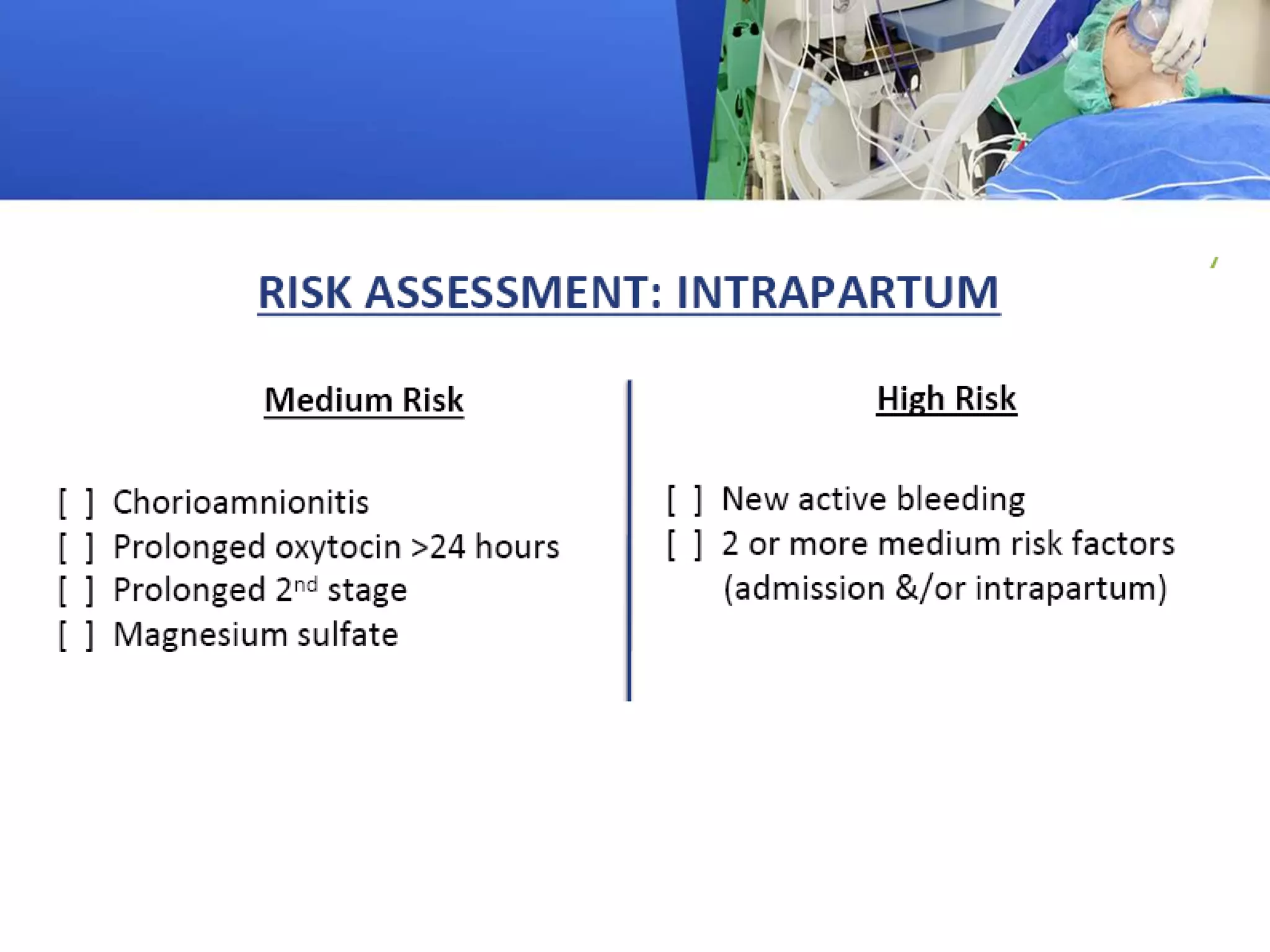
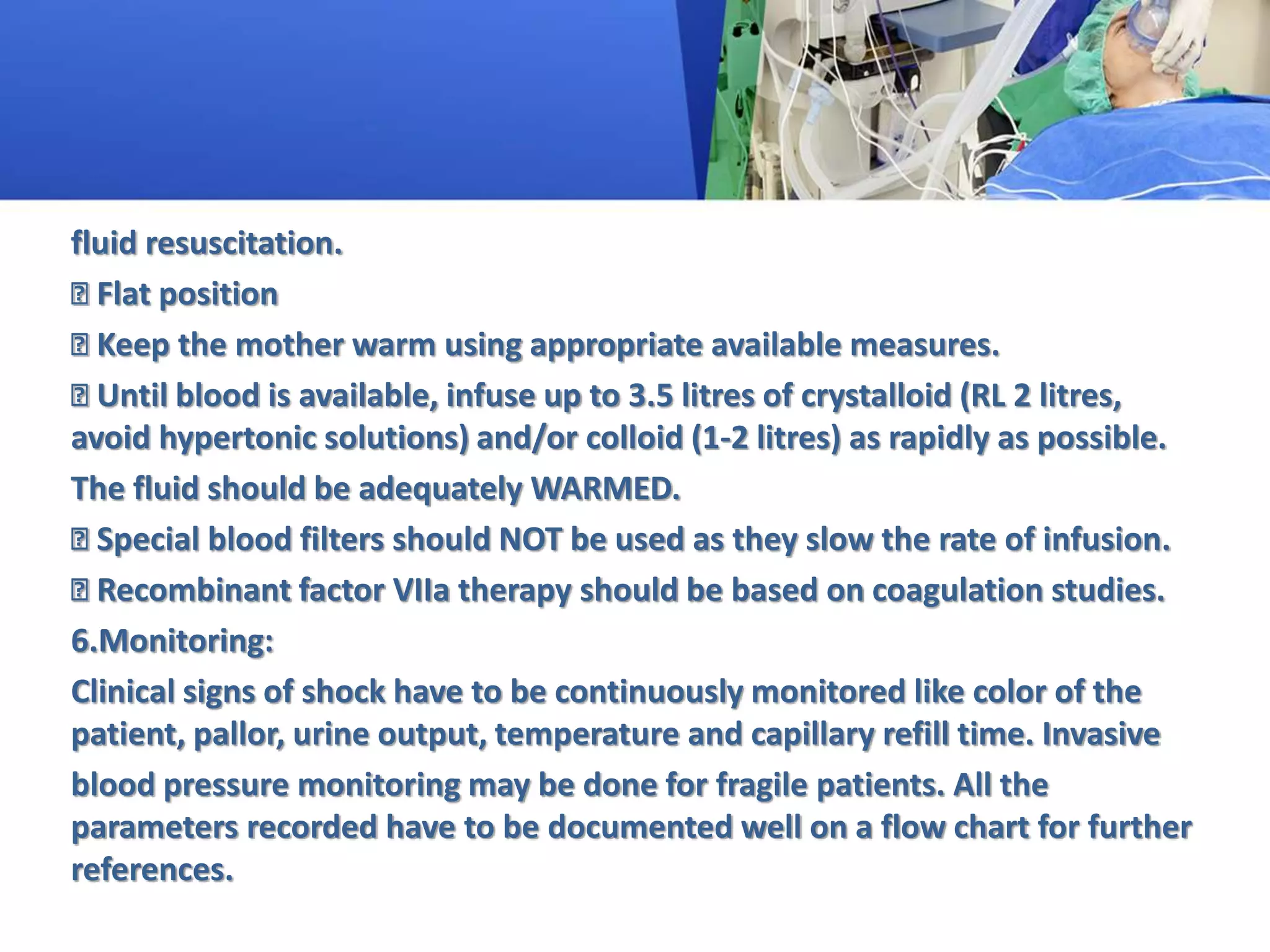
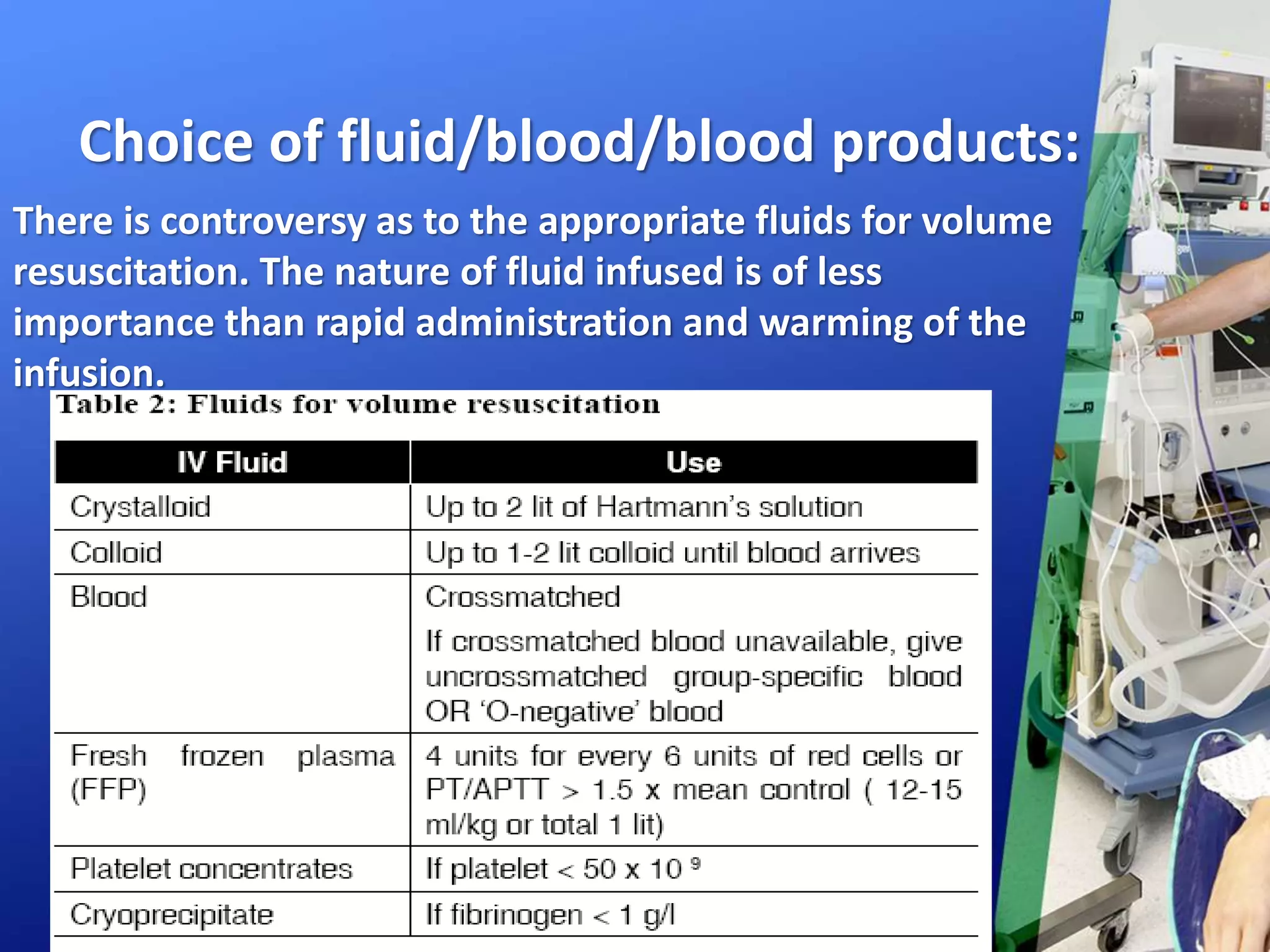
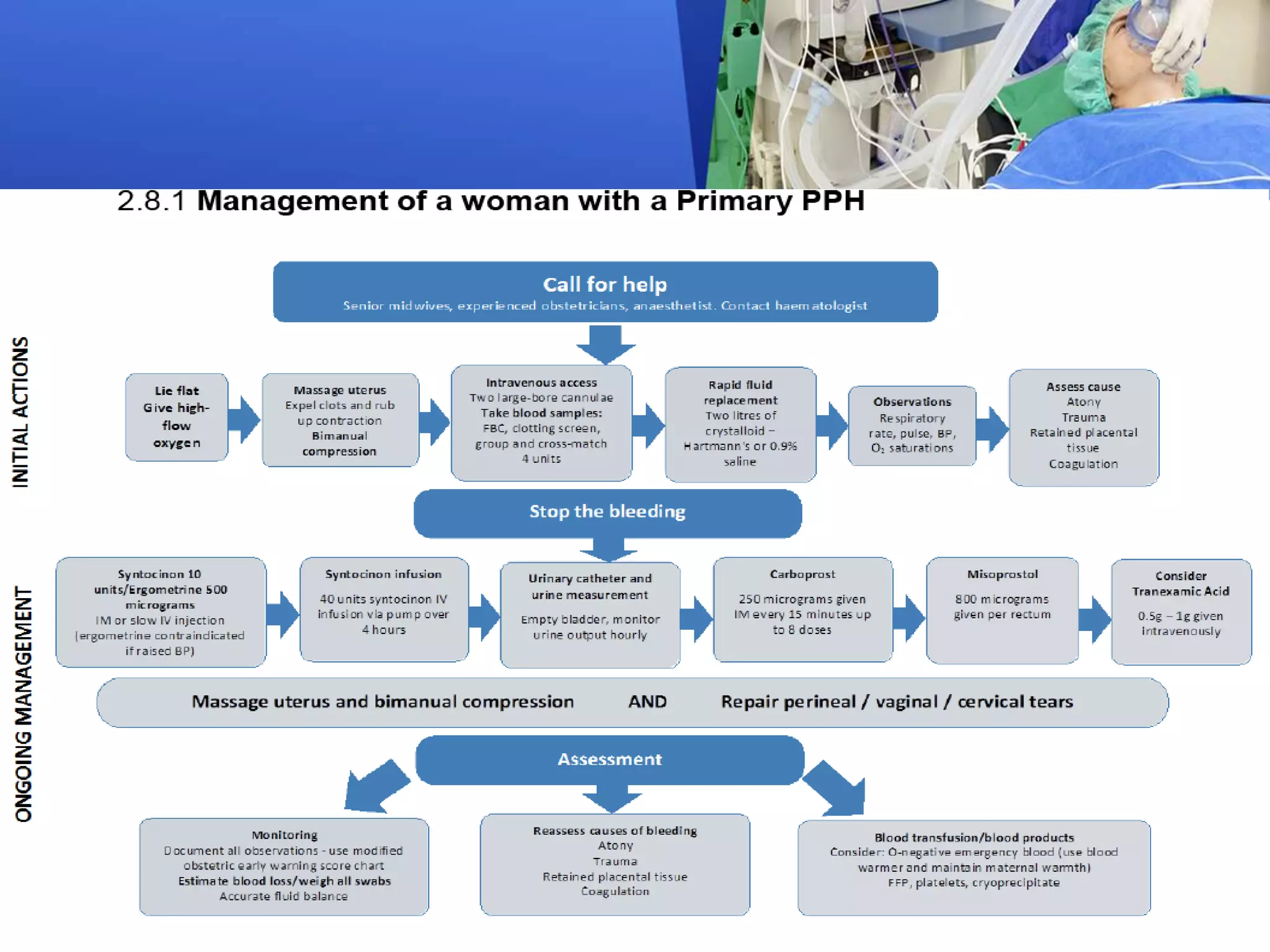
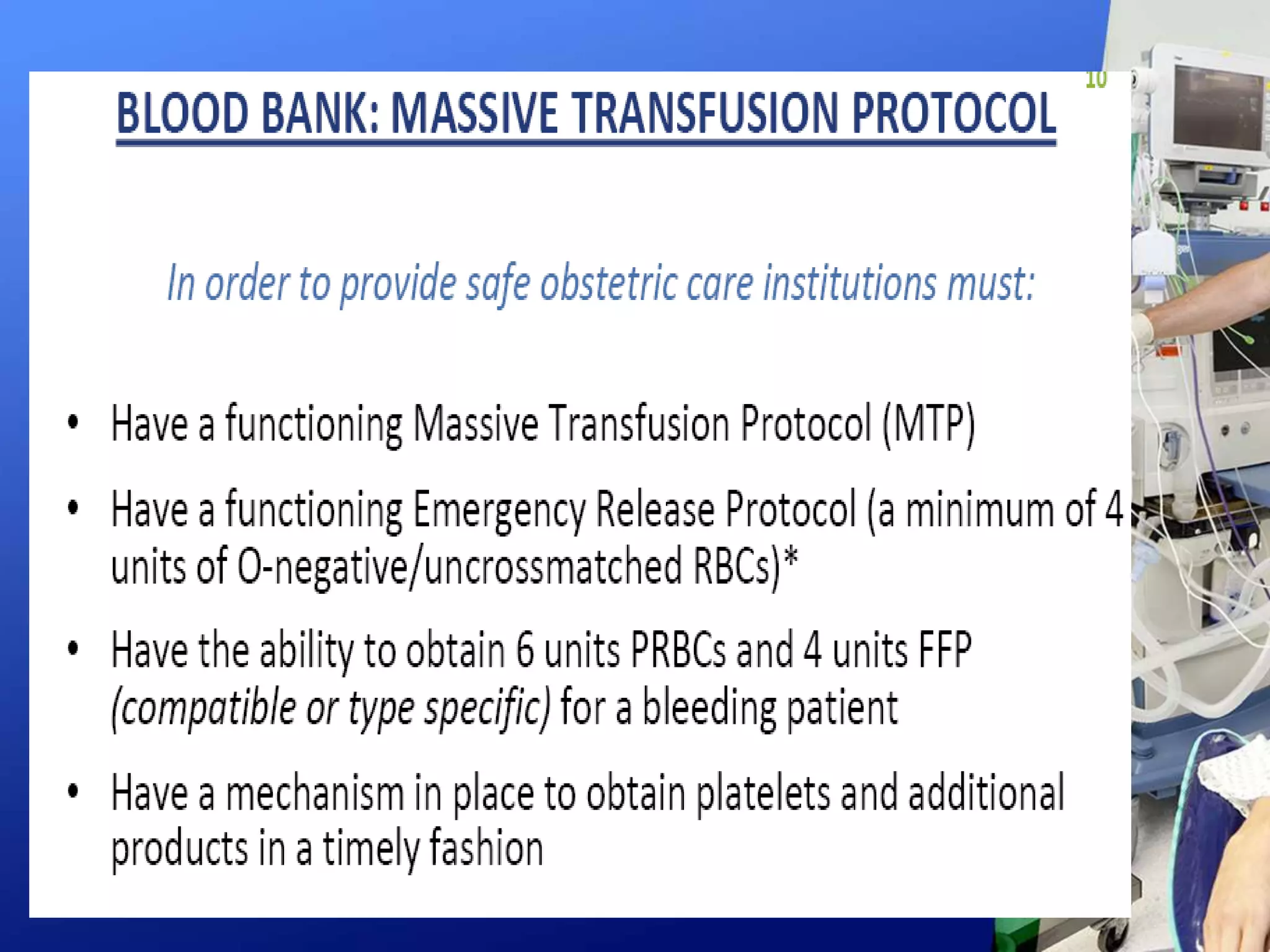
The document outlines the anesthetic implications and management of obstetric hemorrhage, emphasizing the critical role of anesthesiologists in risk assessment, intraoperative communication, and resuscitation protocols. It highlights the importance of continuous monitoring of maternal vital signs and swift administration of blood and fluid replacement, while adhering to guidelines for managing massive blood loss. Additionally, the document discusses the need for readiness, recognition, and response strategies in care settings to improve outcomes for women experiencing obstetric hemorrhage.