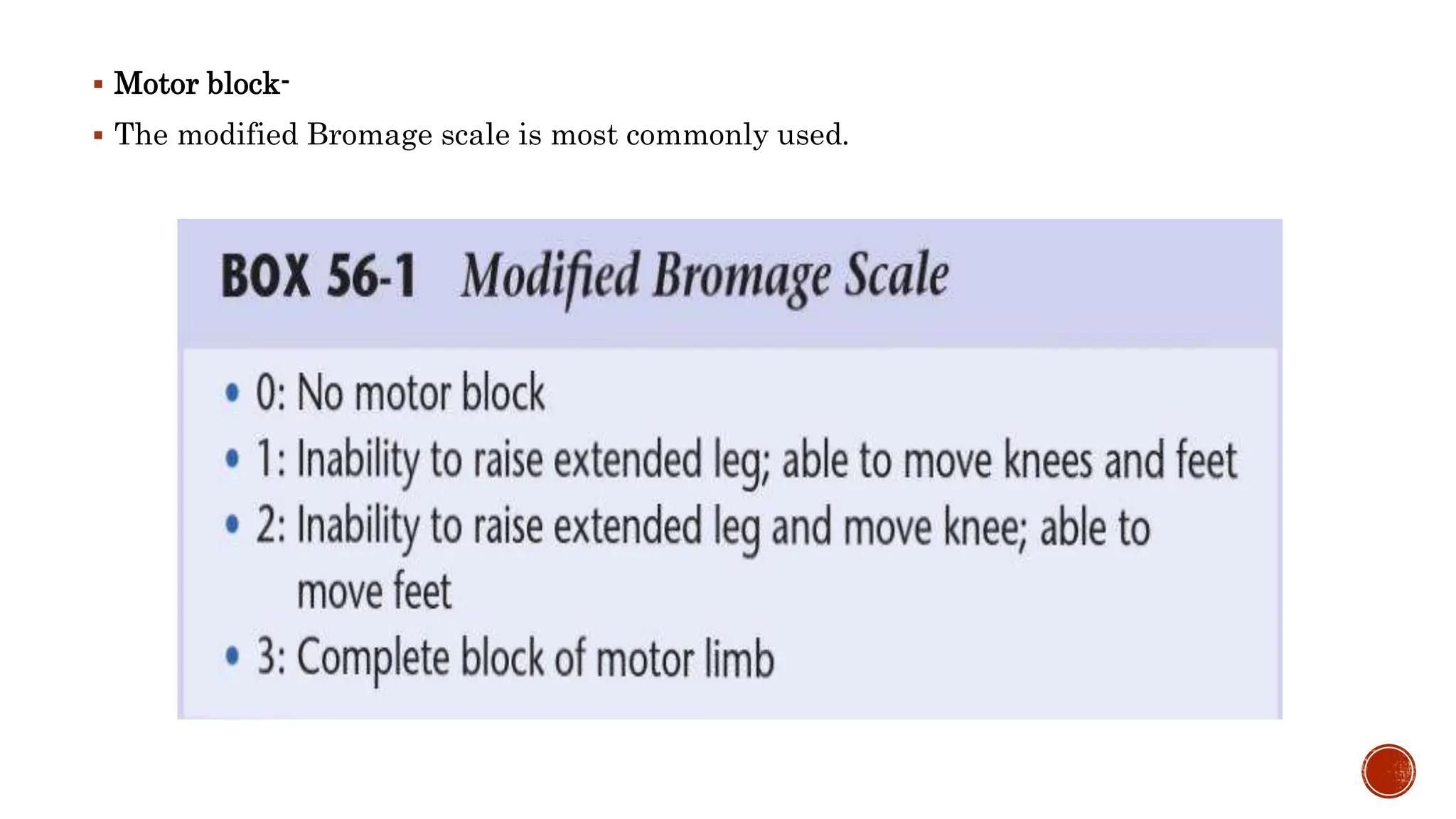
This document discusses spinal anesthesia, including its history, anatomy, physiological effects, indications, contraindications, and various techniques. It highlights the evolution of spinal anesthesia agents, the structure of the spinal cord, the effects on the cardiovascular system, and the factors influencing block height and spread. Additionally, it covers patient positioning, needle types, monitoring during administration, and potential complications associated with neuraxial anesthesia.