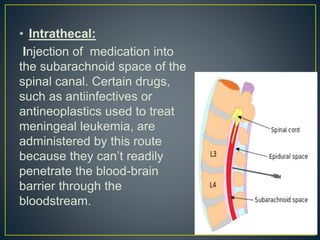
This document discusses epidural and intrathecal administration of medications. It defines epidural administration as injecting medication into the epidural space just outside the subarachnoid space, allowing diffusion into the cerebrospinal fluid. Intrathecal administration injects directly into the subarachnoid space. The document then outlines the proper procedures, equipment, monitoring, and potential complications for epidural administration.