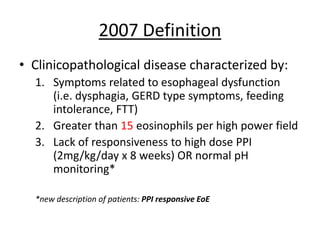
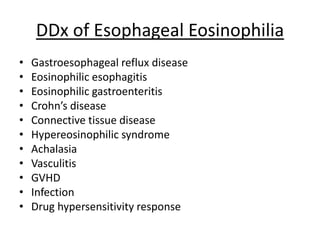
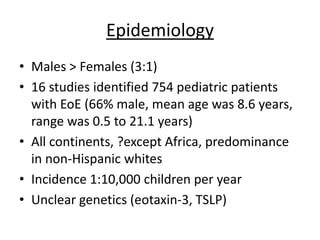
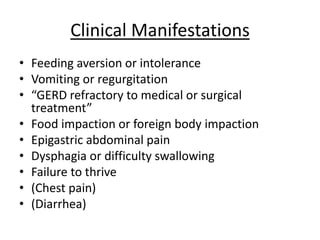
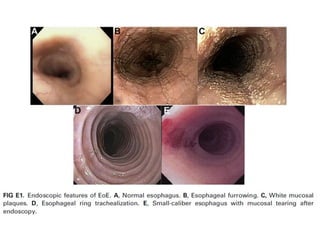
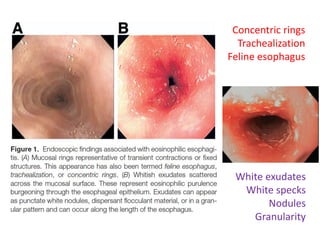
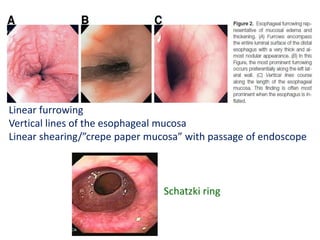
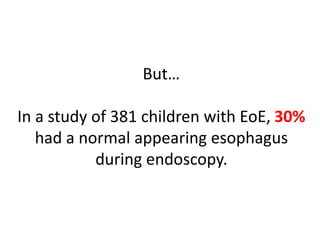
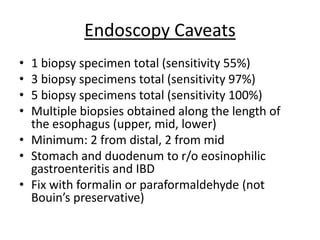
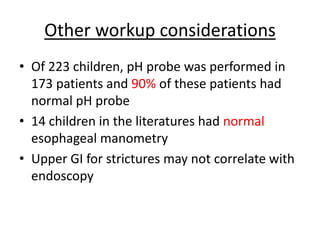
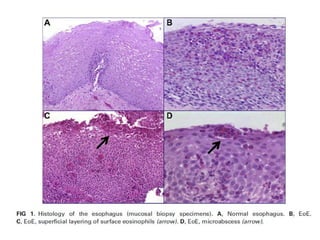
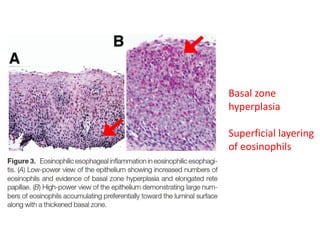
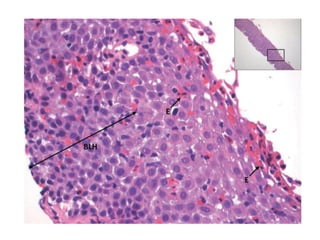
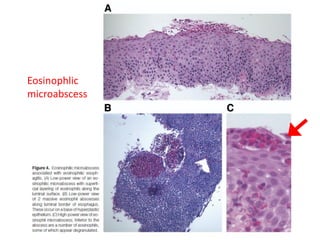
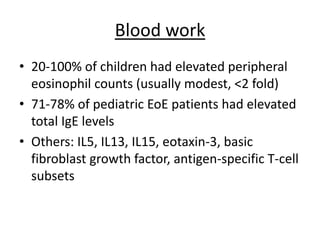
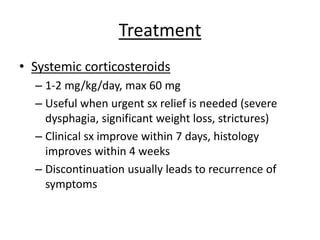
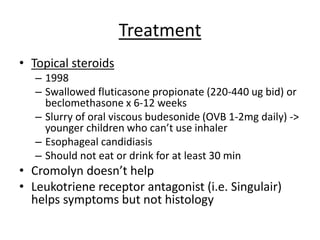
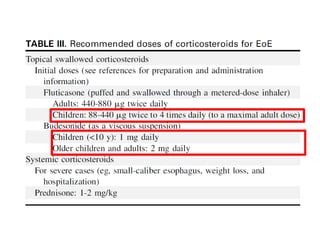
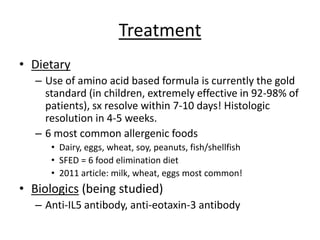
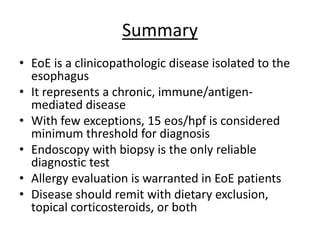
Eosinophilic esophagitis (EoE) is a chronic immune/antigen-mediated disease characterized by esophageal dysfunction symptoms and >15 eosinophils per high power field in esophageal biopsies. It was first reported in 1977. Diagnosis requires ruling out GERD and involves endoscopy with multiple biopsies. Treatment includes topical steroids, dietary elimination, or systemic steroids to reduce symptoms and support tissue healing. EoE affects males more than females and tends to be a relapsing condition requiring long-term management.