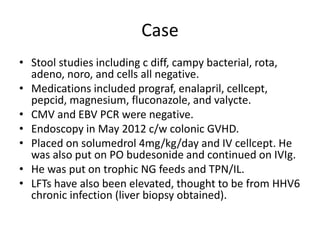
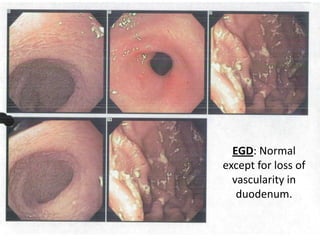
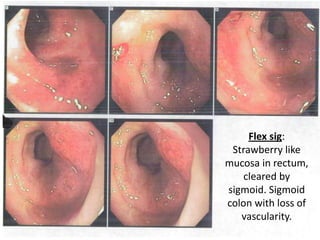
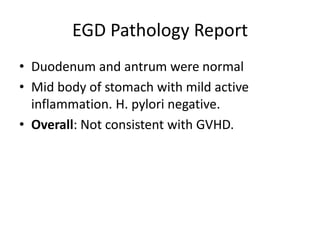
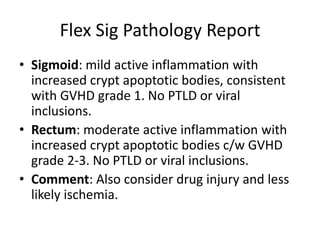
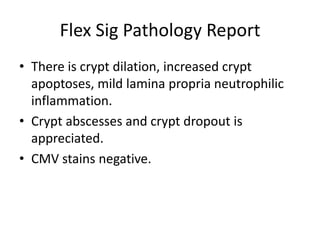
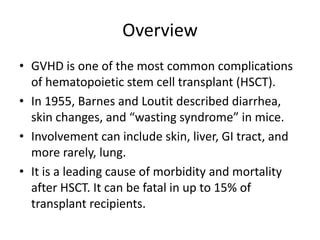
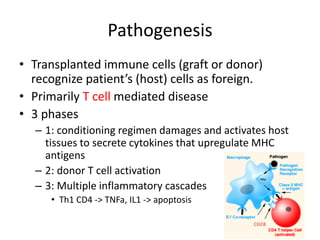
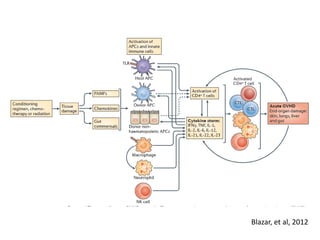
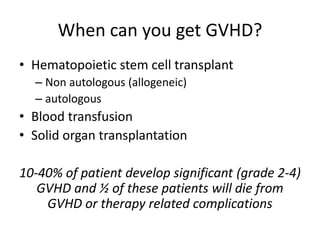
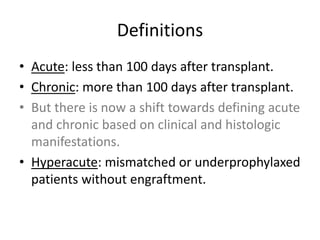
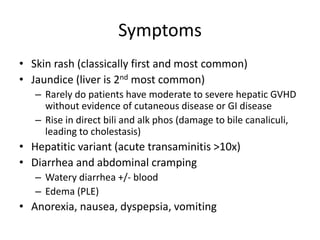
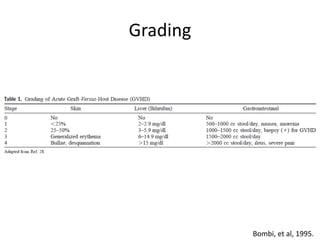
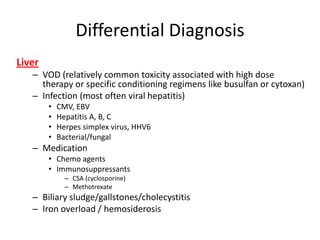
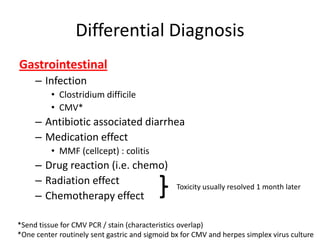
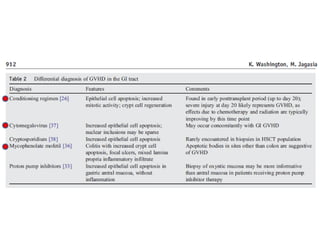
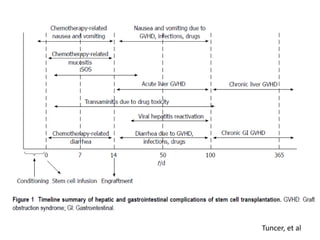
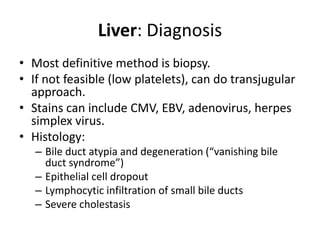
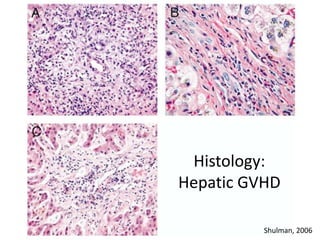
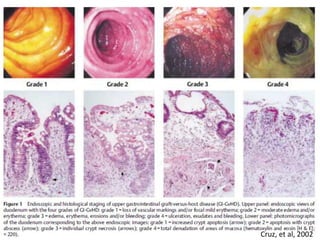
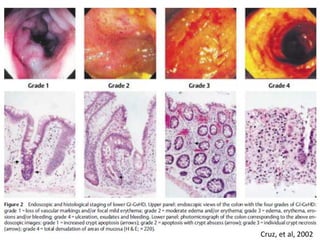
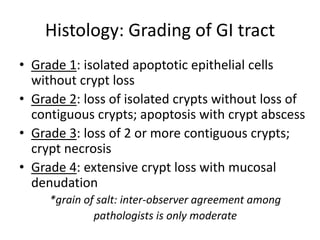
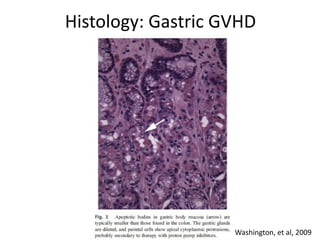
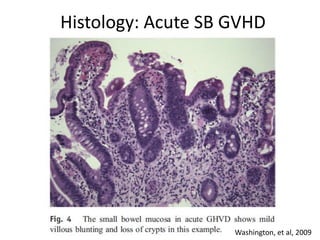
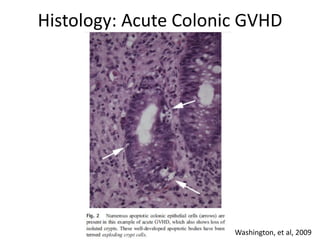
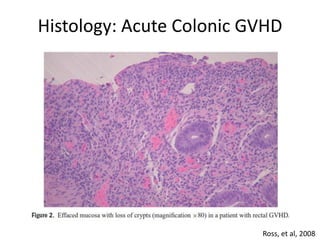
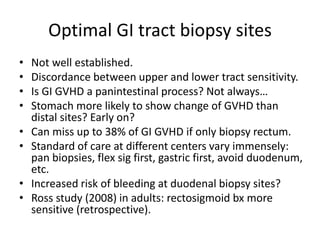
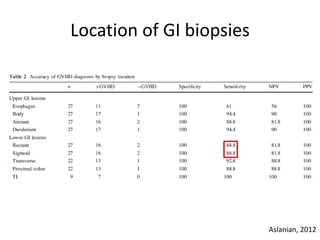
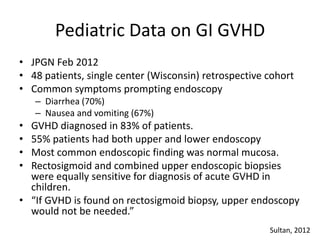
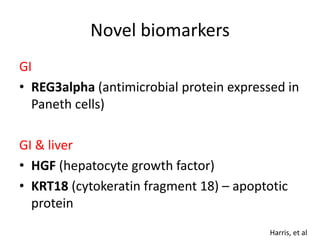
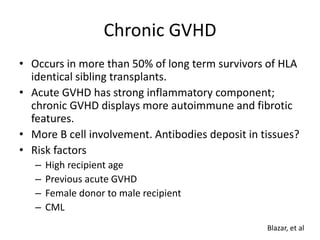
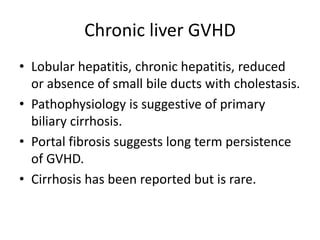
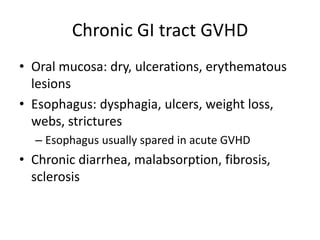
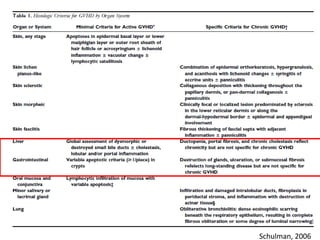
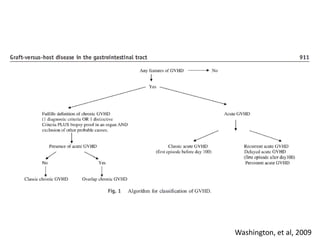
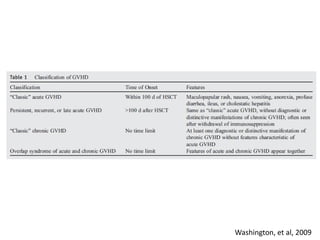
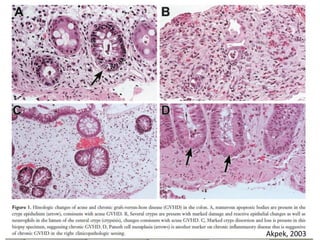
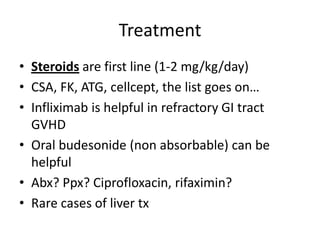
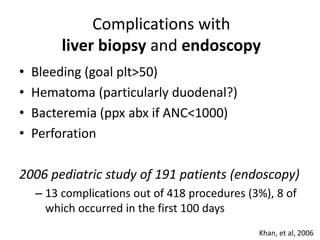
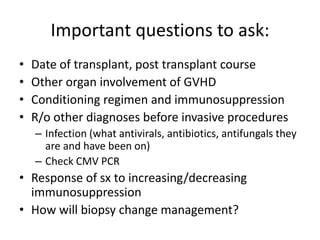
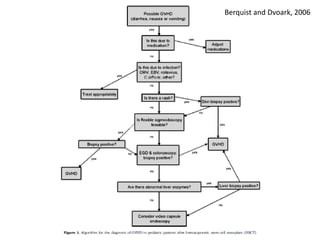
This document discusses gastrointestinal and liver graft versus host disease (GVHD) in pediatric patients. It begins with an overview of GVHD, including definitions, pathogenesis, risk factors, symptoms, grading scales, and differential diagnoses for liver and GI involvement. The case presentation describes a 22 month old boy with skin and GI GVHD following a bone marrow transplant. Endoscopy findings and biopsy results are discussed which supported a diagnosis of colonic GVHD. Histologic characteristics of acute and chronic GI and liver GVHD are reviewed. Optimal biopsy sites and challenges in diagnosis are also covered.