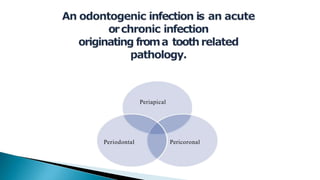
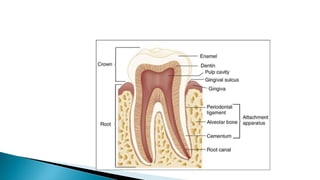
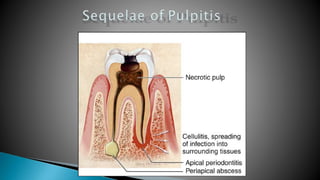
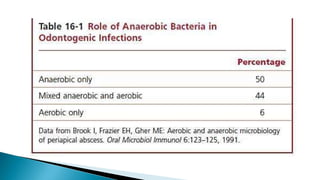
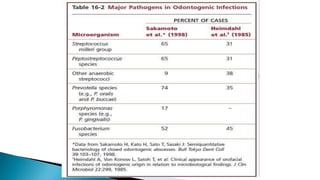
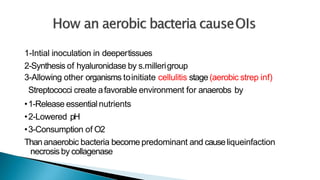
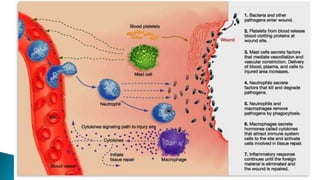
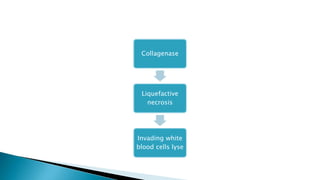
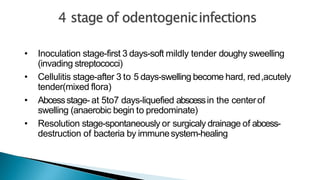
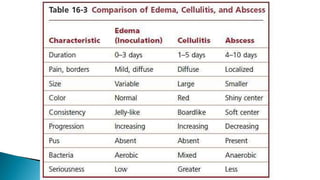
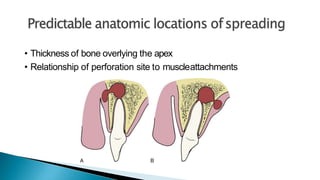
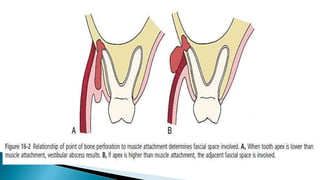
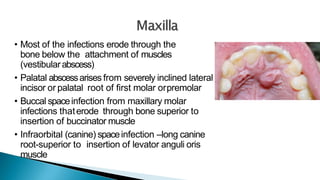
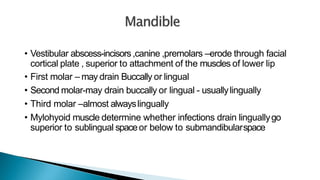
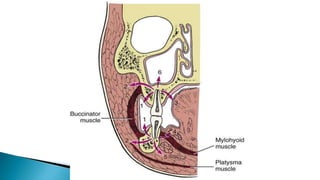
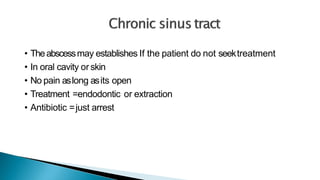
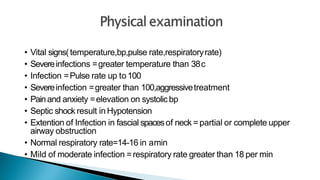
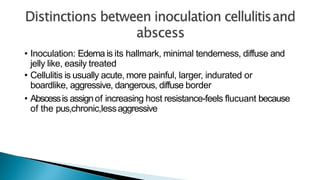
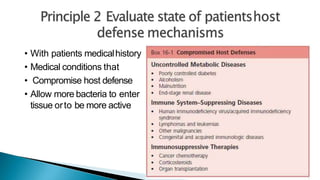
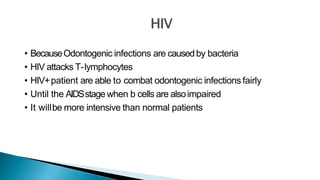
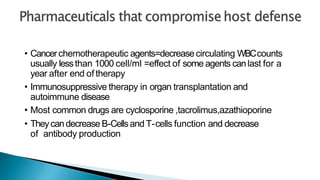
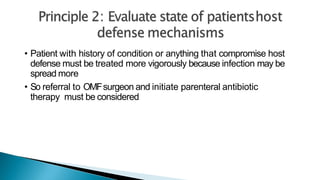
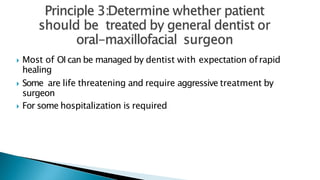
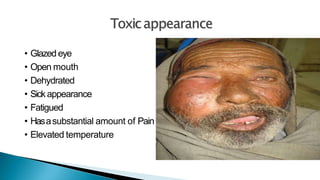
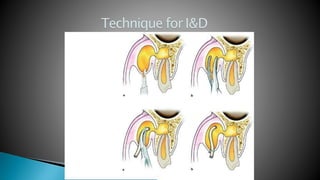
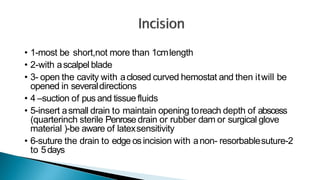
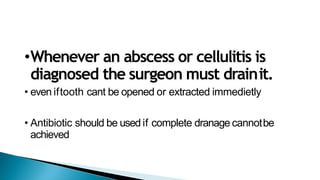
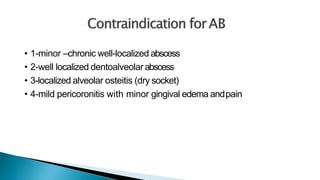
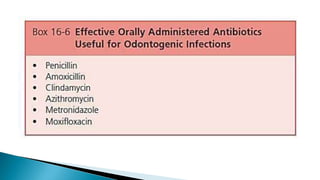
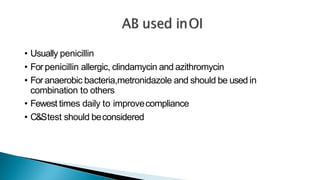
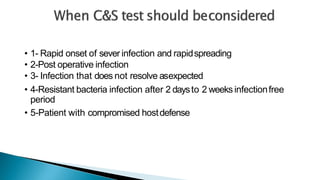
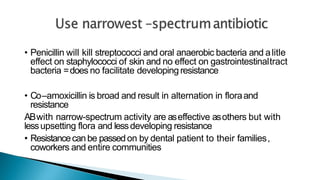
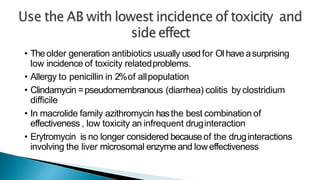
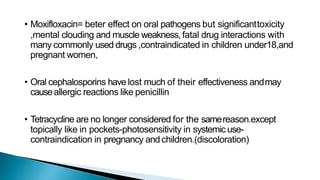
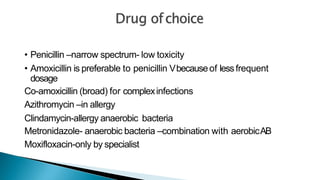
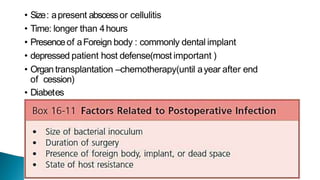
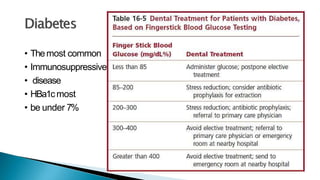
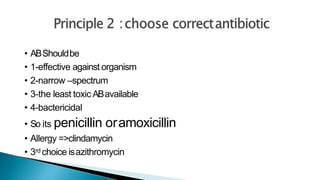
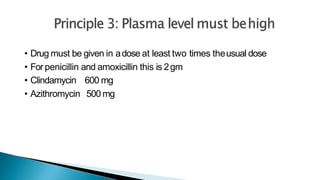
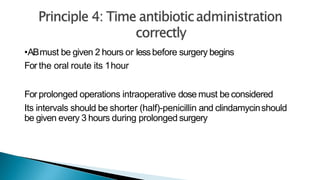
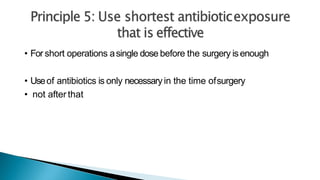
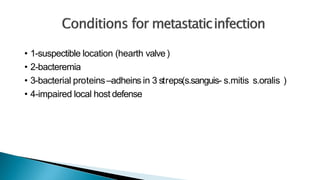
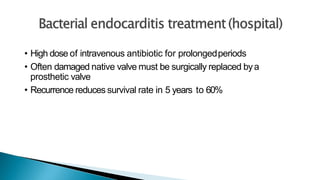
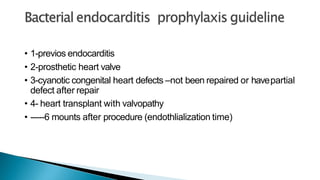
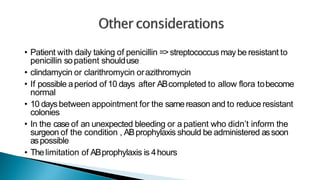
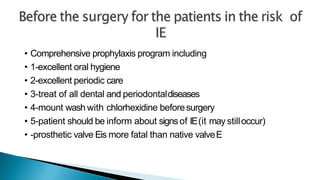
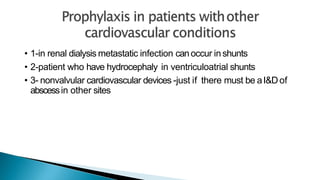
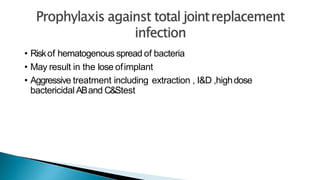
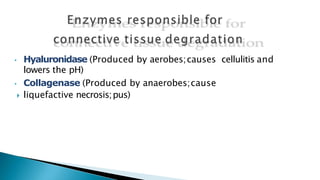
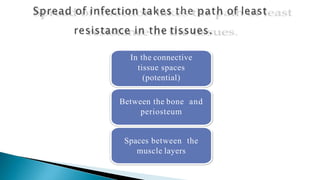
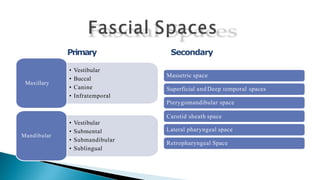
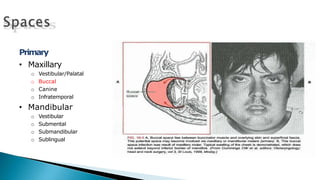
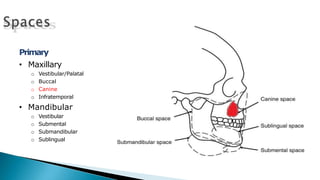
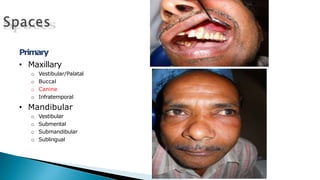
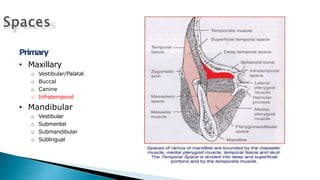
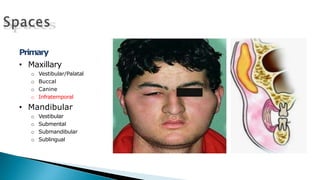
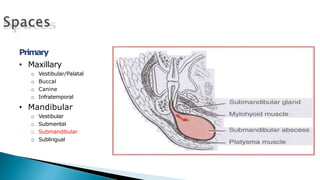
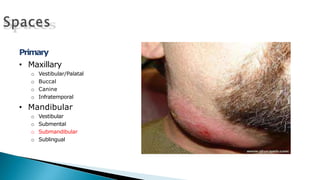
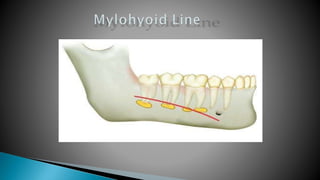
The document discusses odontogenic infections, detailing their causes, symptoms, stages, diagnostic methods, and treatment options, emphasizing the role of various bacteria. It highlights the importance of surgical intervention and appropriate antibiotic therapy, particularly for immunocompromised patients. It also outlines specific infection management strategies and the necessity for referral to specialists in severe cases.