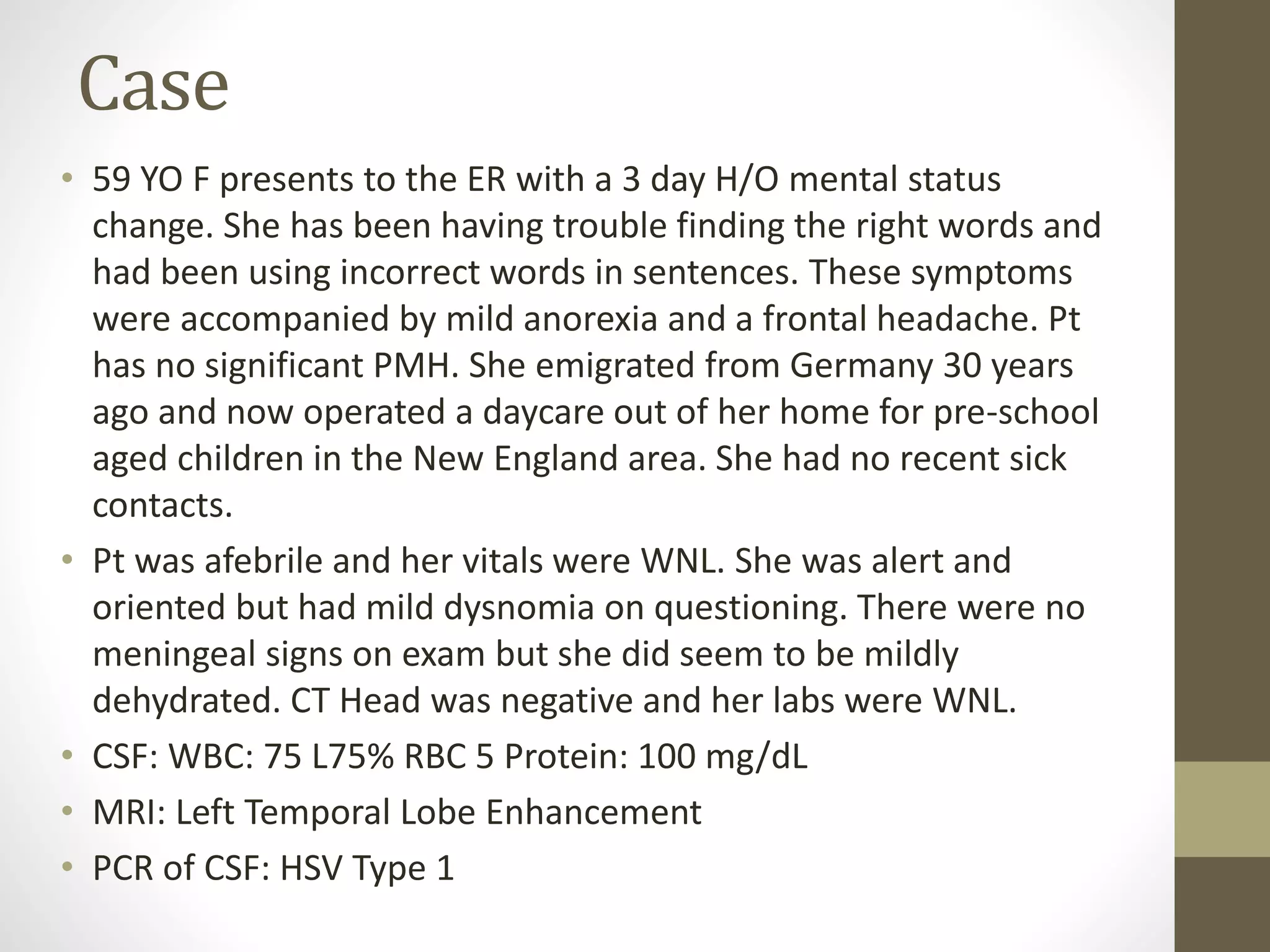
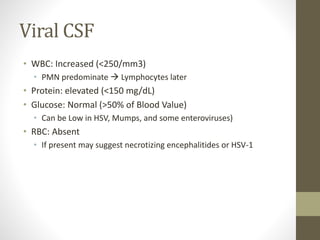
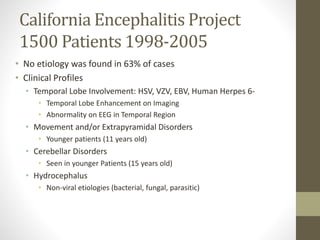
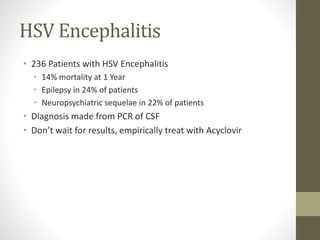
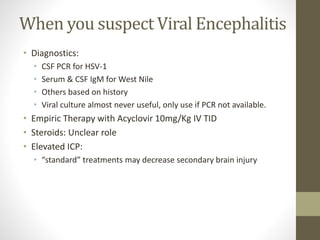
A 59-year-old German woman presented to the ER with symptoms of mental status changes including difficulty finding words and using incorrect words over the past 3 days, accompanied by mild loss of appetite and headache. Tests revealed inflammation in the brain and meninges, with HSV Type 1 detected in her cerebrospinal fluid by PCR. Her symptoms, MRI findings of left temporal lobe enhancement, and CSF profile were consistent with her diagnosis of herpes simplex virus encephalitis.