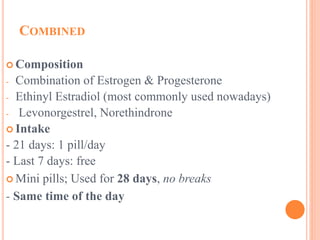
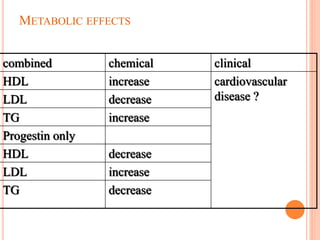
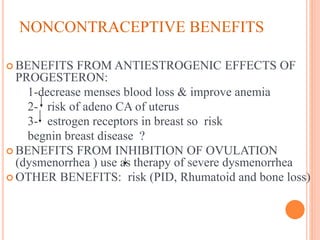
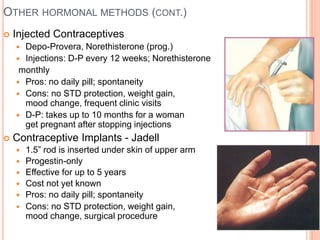
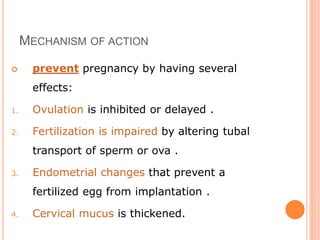
This document discusses various contraceptive methods including natural, barrier, hormonal, and intrauterine devices. It focuses on hormonal contraception, describing how different hormonal methods work to prevent ovulation and fertilization. The main hormonal contraceptives discussed are oral contraceptive pills containing estrogen and progestin, as well as emergency contraceptive pills containing just progestin. The document outlines the types of oral contraceptive pills, how they work, possible side effects, benefits and risks. Emergency contraceptive pills are described as a backup method to prevent pregnancy after unprotected intercourse.