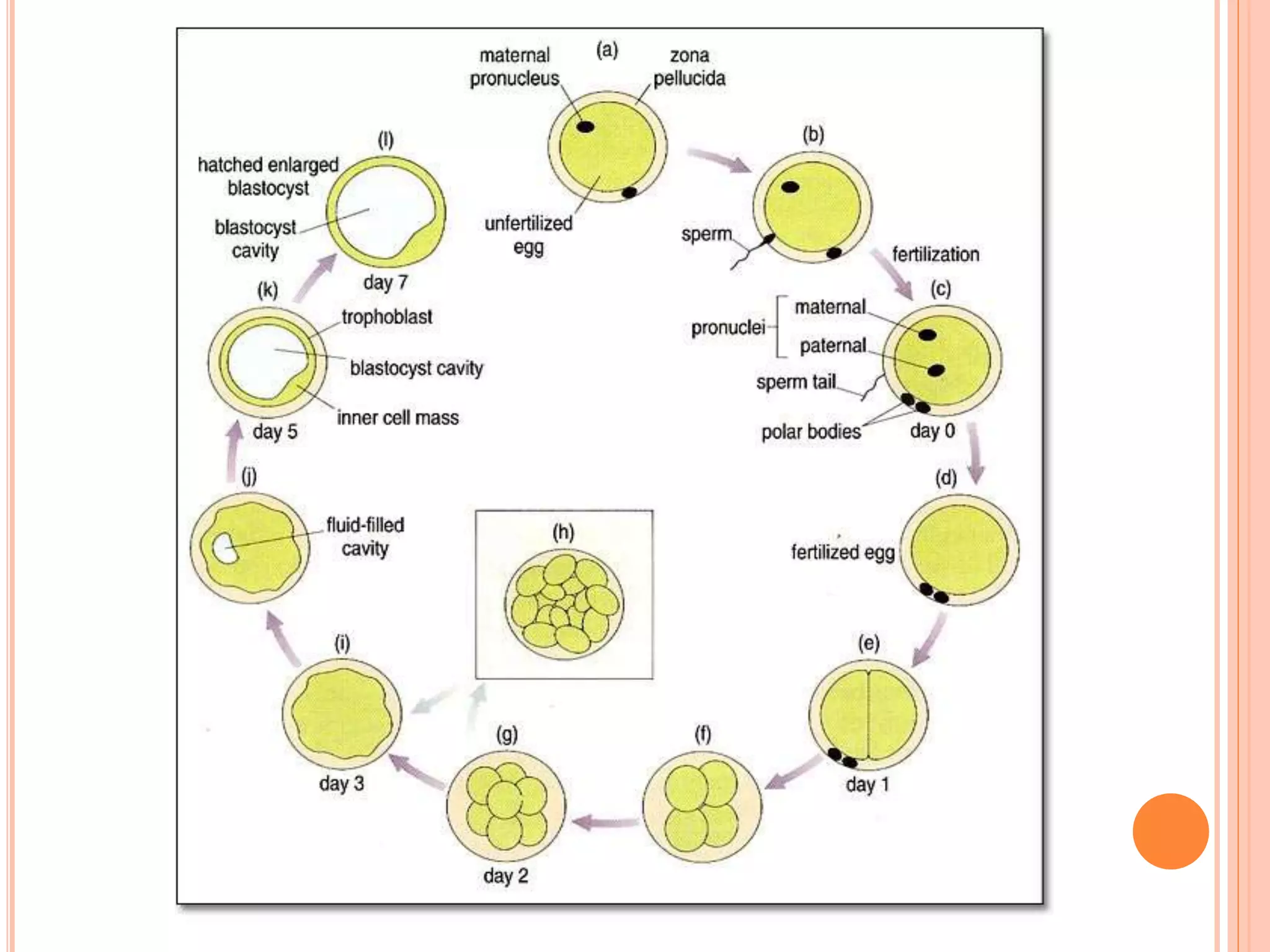
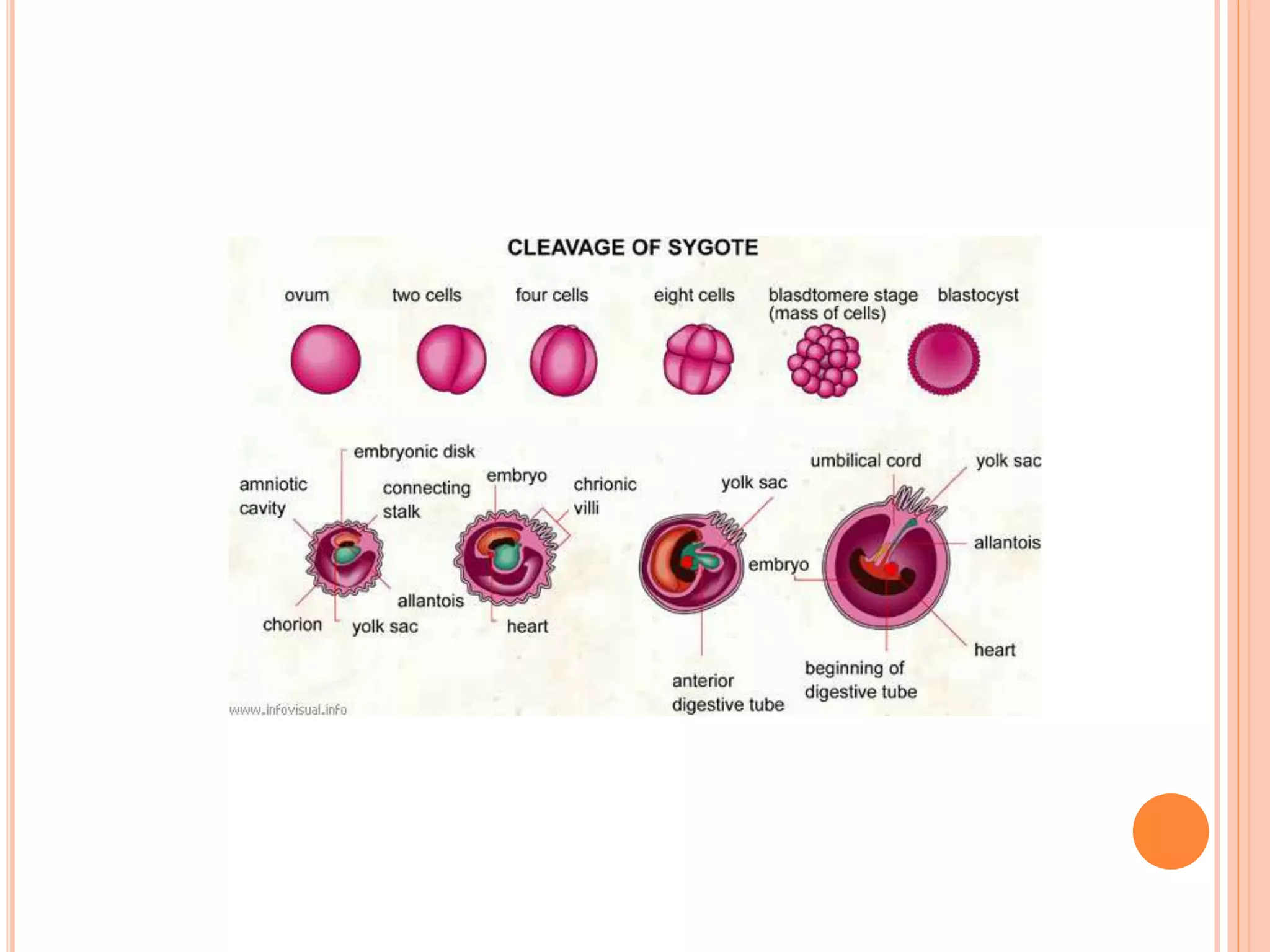
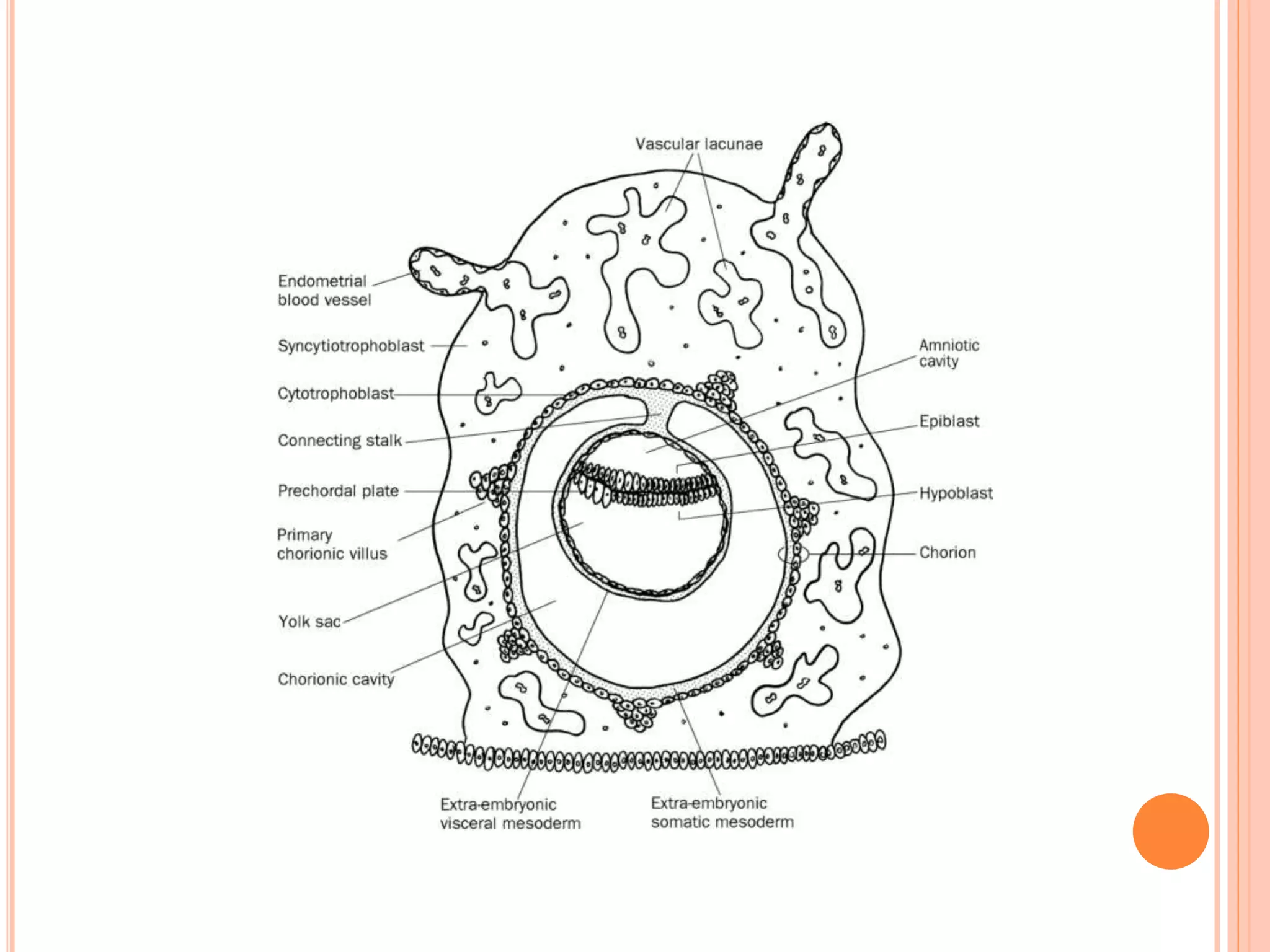
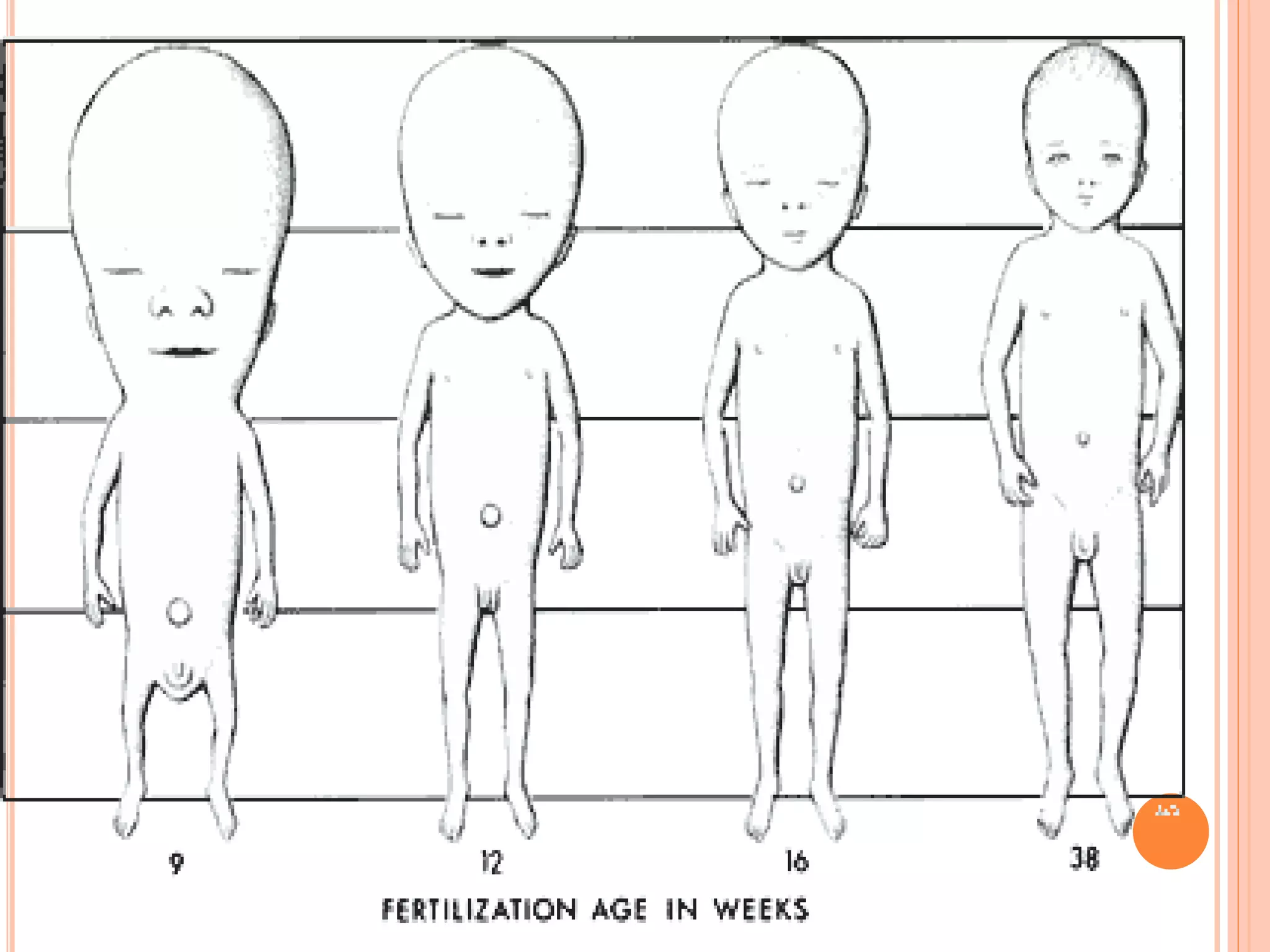
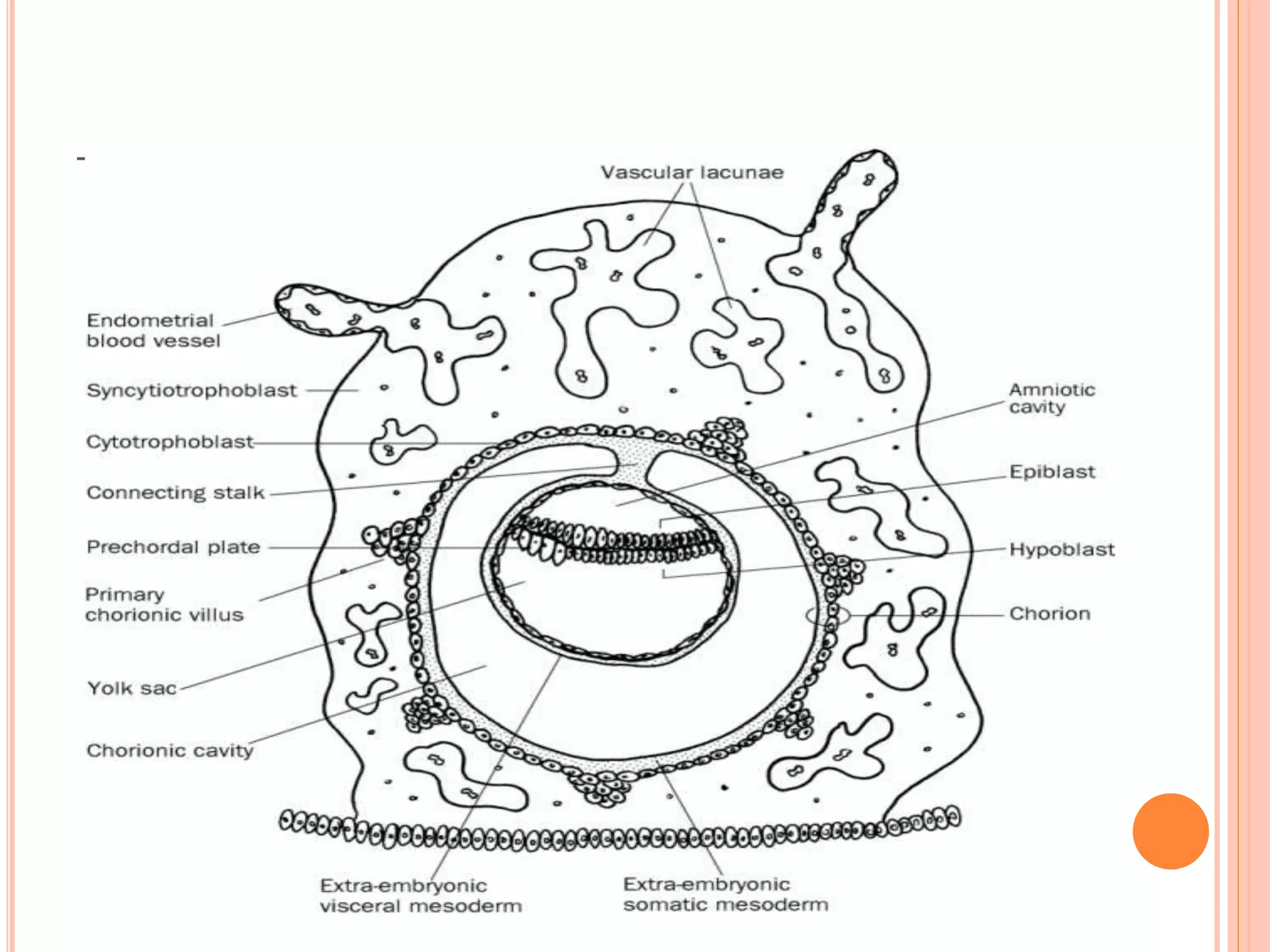
Embryology studies the changes occurring from fertilization to adulthood, focusing on prenatal development. It encompasses two main aspects: ontogeny (individual development) and phylogeny (evolutionary history), and it introduces essential concepts like zygote, morula, implantation, and embryo. Understanding embryology helps clarify human developmental processes and their implications for various medical fields, including obstetrics and pathology.