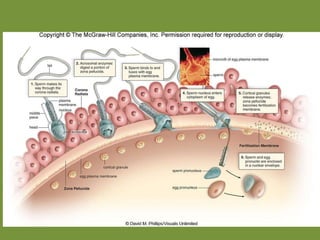
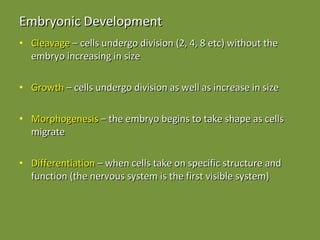
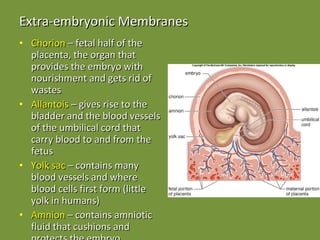
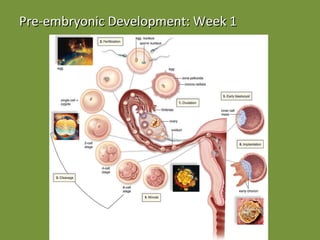
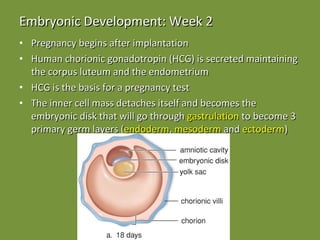
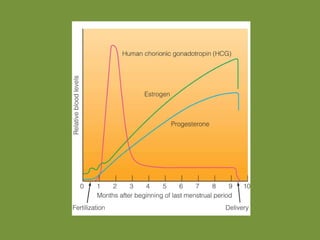
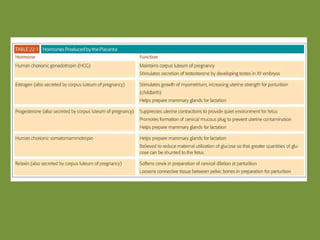
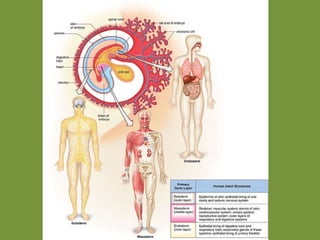
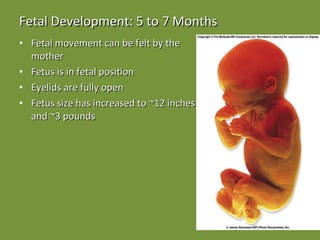
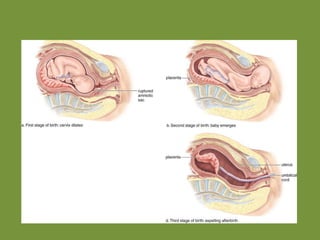
Fertilization involves the union of an egg and sperm to form a zygote. The sperm penetrates layers surrounding the egg and fuses with the egg's membrane. The sperm and egg nuclei then fuse. The egg's membrane then changes to prevent additional sperm from entering. During embryonic development, cells undergo cleavage and differentiation, forming the three primary germ layers. Fetal development occurs over nine months as organs grow and body systems develop fully. Birth occurs in three stages as the cervix dilates, the child is delivered, and the placenta is expelled.