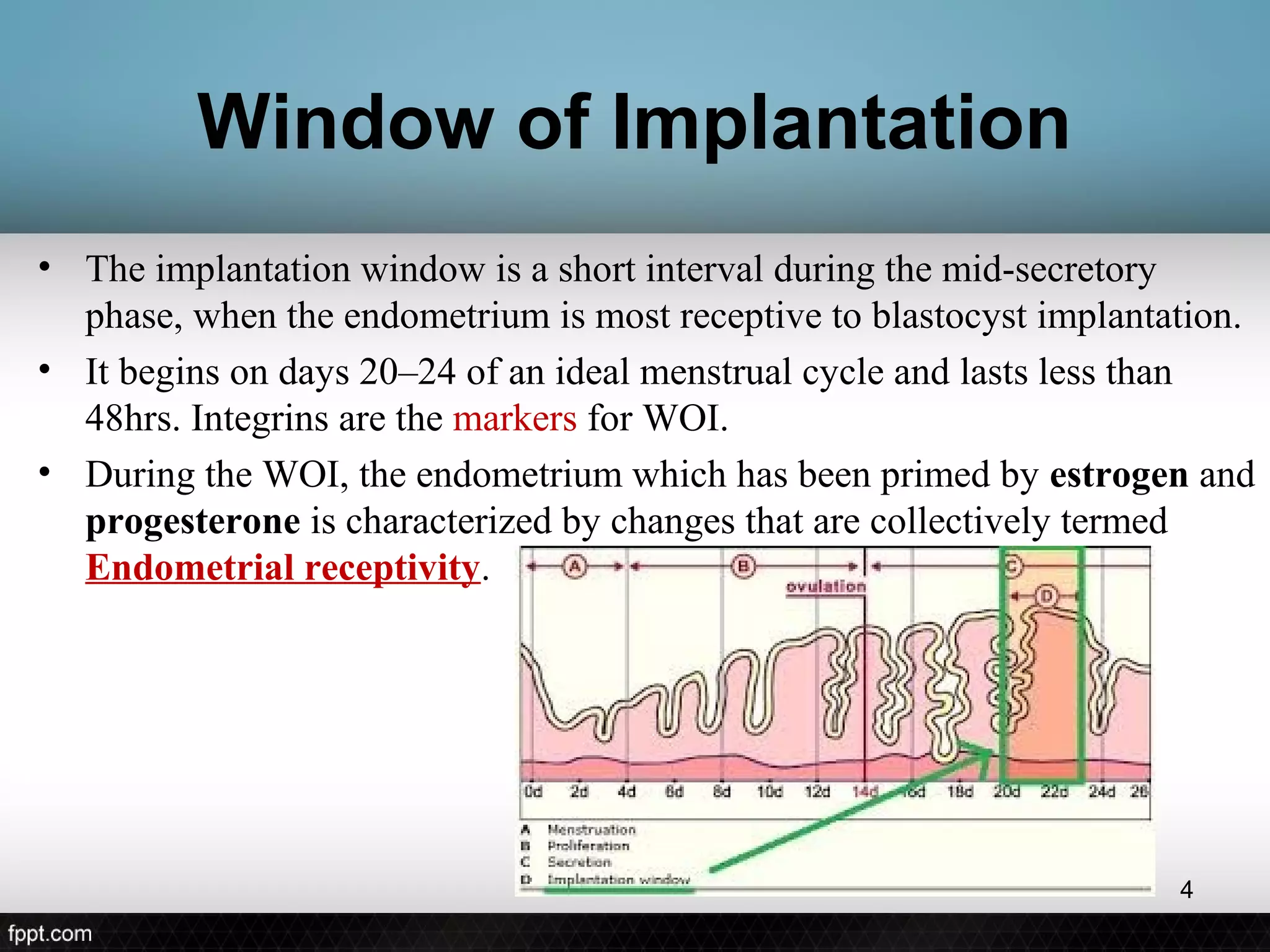
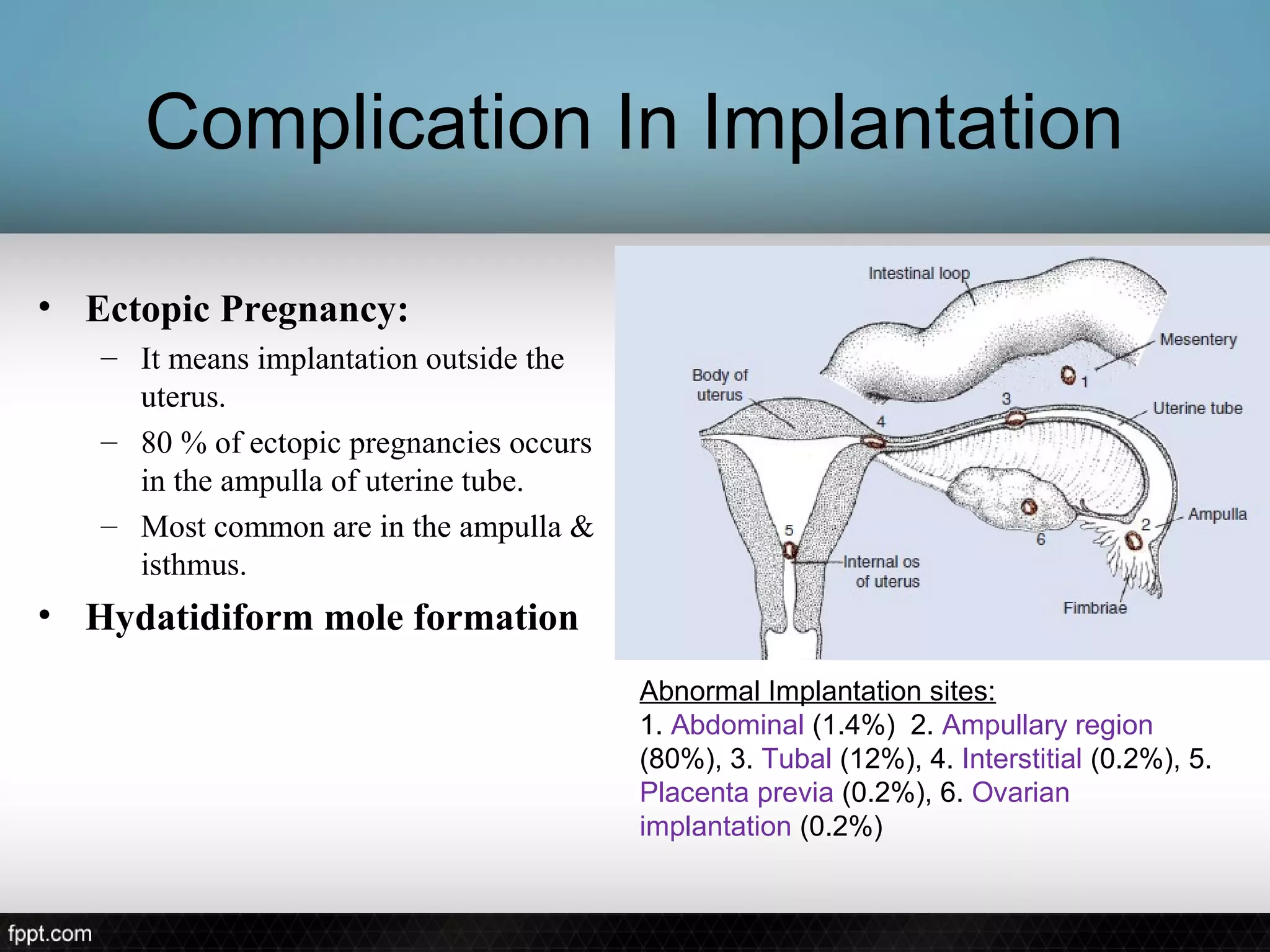
The document discusses the process of implantation, beginning with definitions and timing. Implantation occurs around 6 days after fertilization and is completed by 11 days. The blastocyst implants in the posterior uterine wall. There is a short window of implantation around days 20-24 of the menstrual cycle. During this time, pinopods appear on the endometrial surface and decidualization of the endometrial stroma occurs to support implantation. The stages of implantation are apposition, adhesion, and invasion of the trophoblast into the endometrium. Various mediators help guide the blastocyst to the optimal implantation site. Complications can include ectopic pregnancy and abnormal placentation.