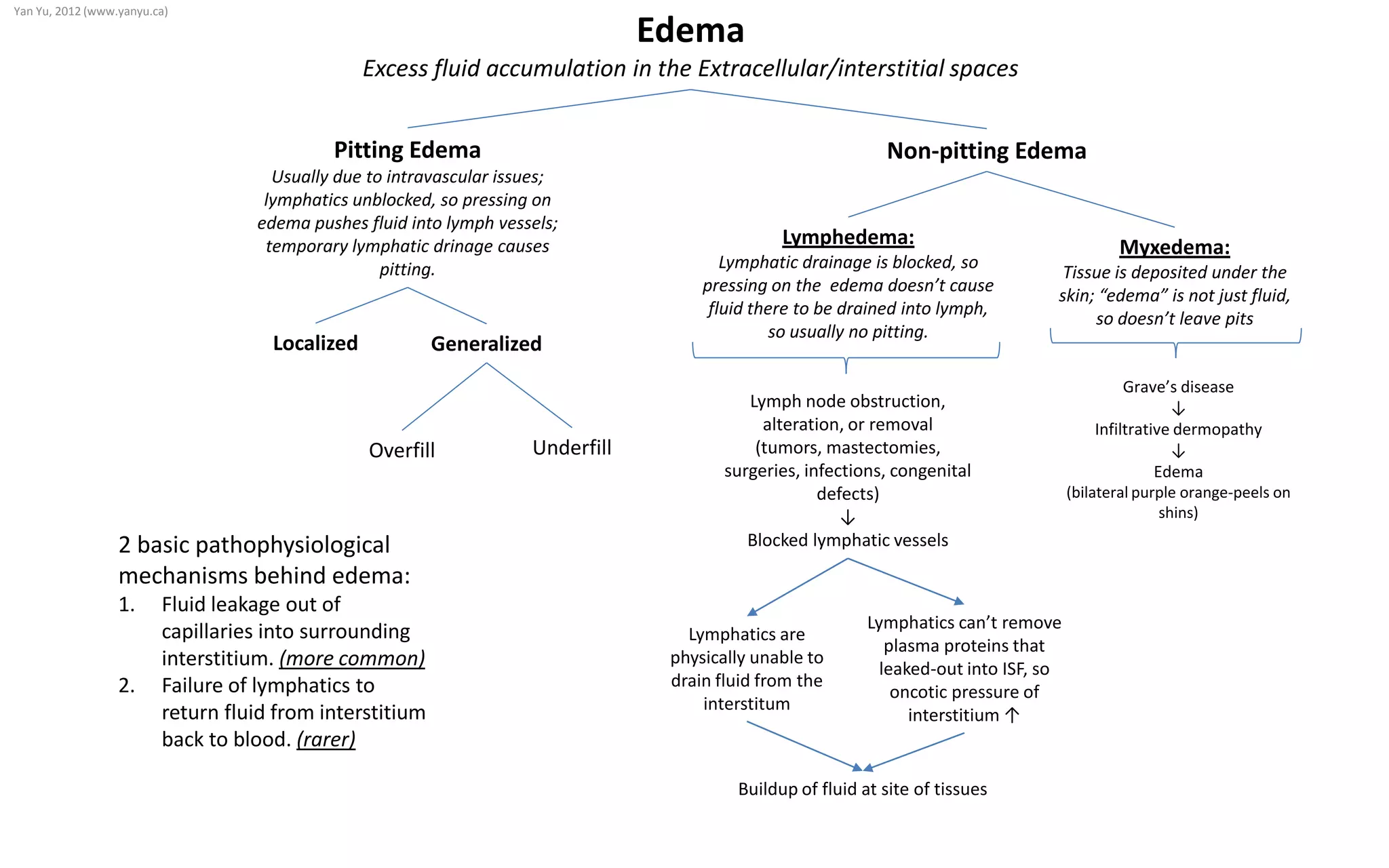
Lymphedema is caused by blocked lymphatic drainage, which prevents fluid from being drained from tissues into lymph vessels. This results in non-pitting edema, as pressing on the swollen area does not cause indentations since fluid cannot be pushed into blocked lymphatics. Pitting edema is usually due to issues within blood vessels and occurs when lymphatics are unblocked, allowing pressing on the swollen area to temporarily drain fluid into lymphatic vessels, forming indentations. There are two main causes of edema: 1) fluid leakage from capillaries into tissues, and 2) failure of lymphatics to return fluid from tissues back to the bloodstream. Lymphedema occurs when lymph nodes