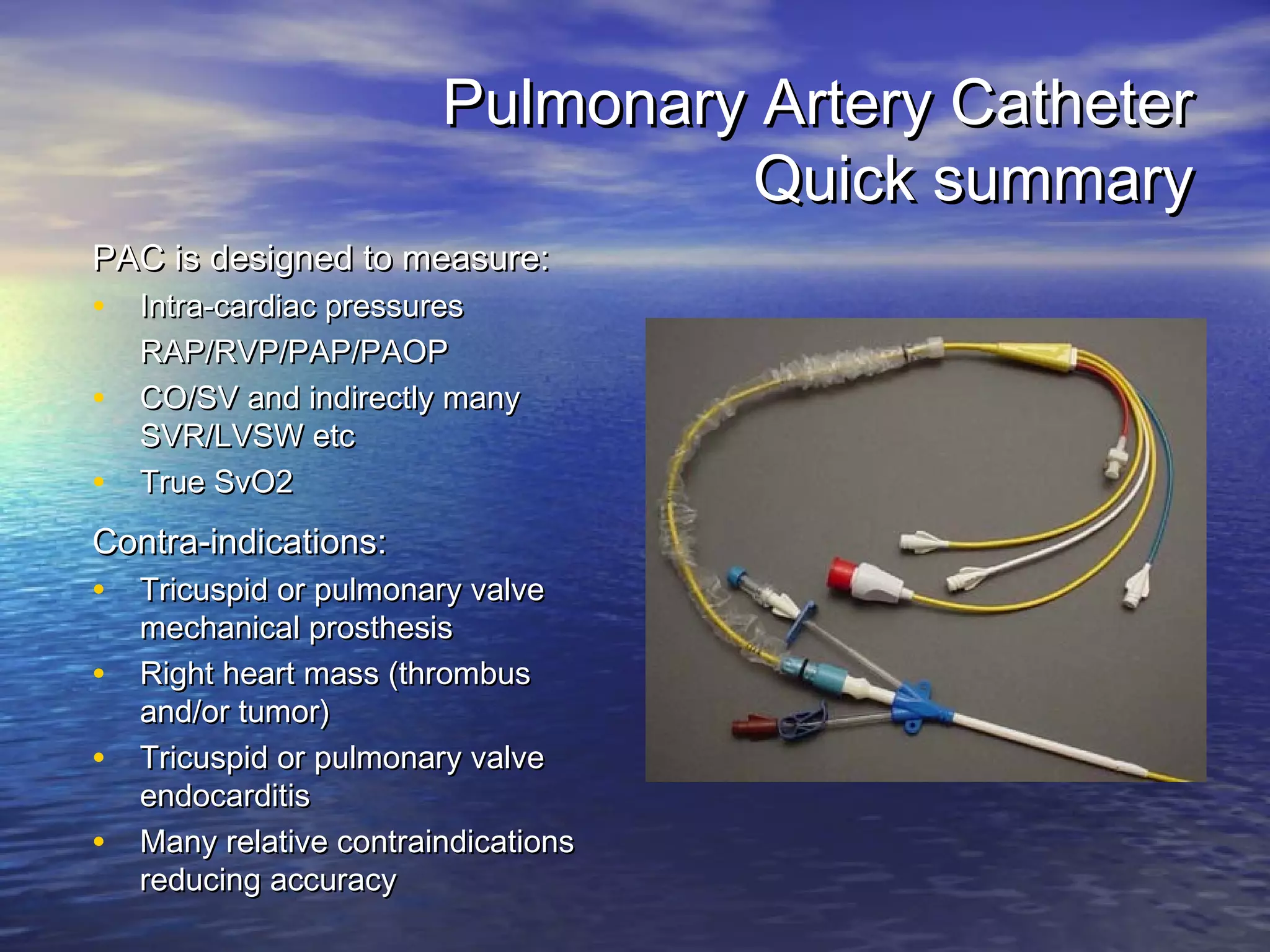
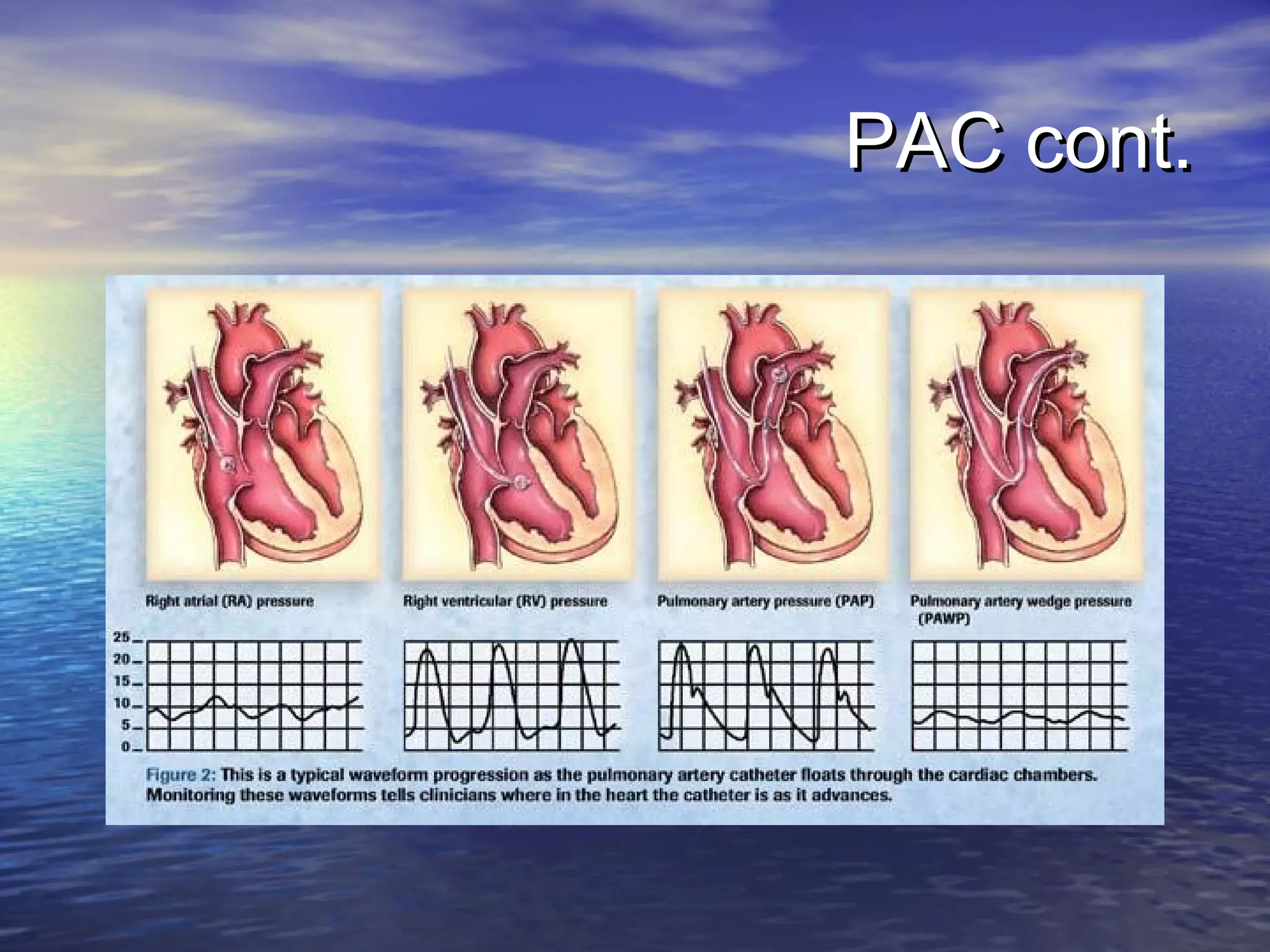
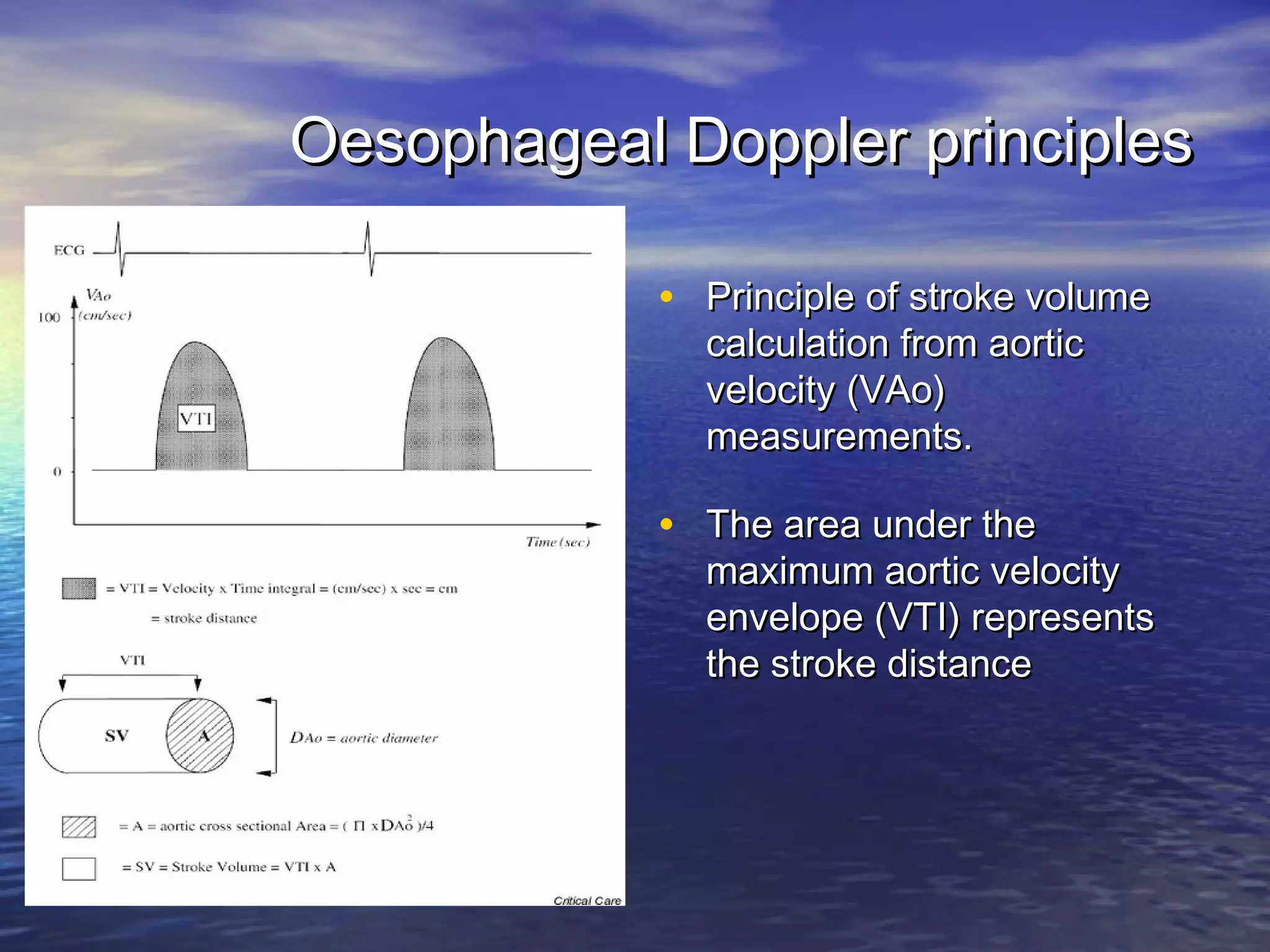
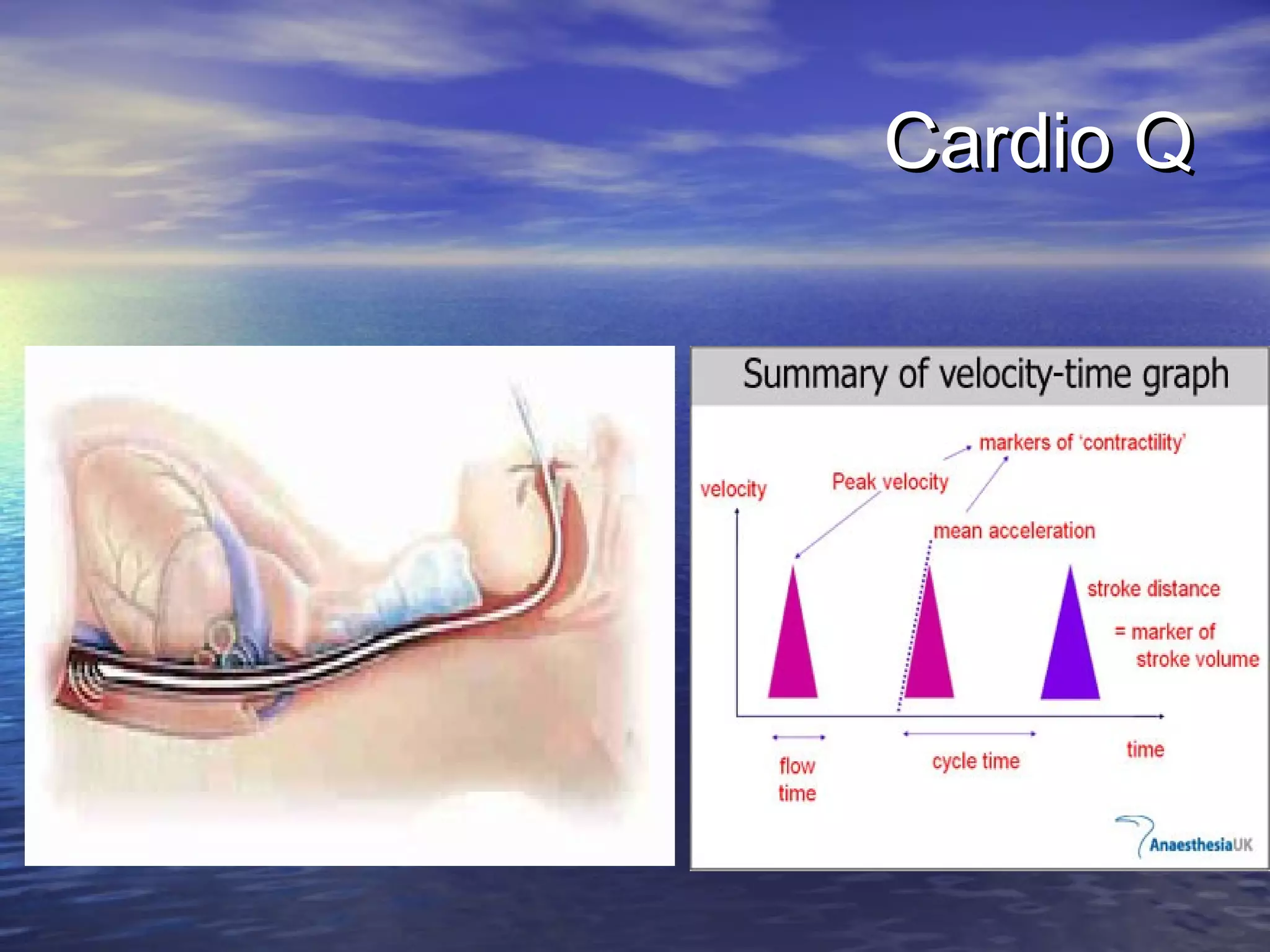
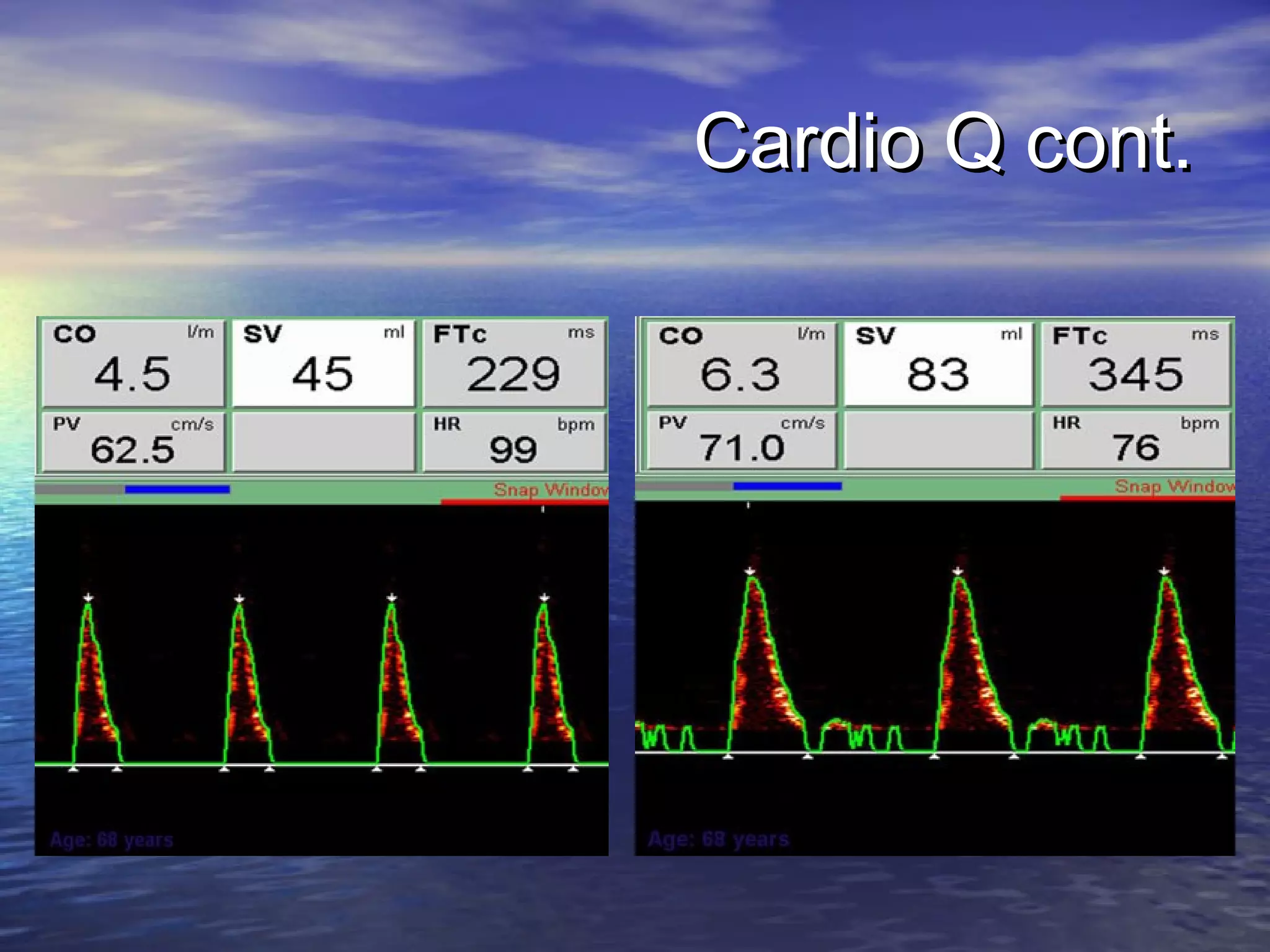
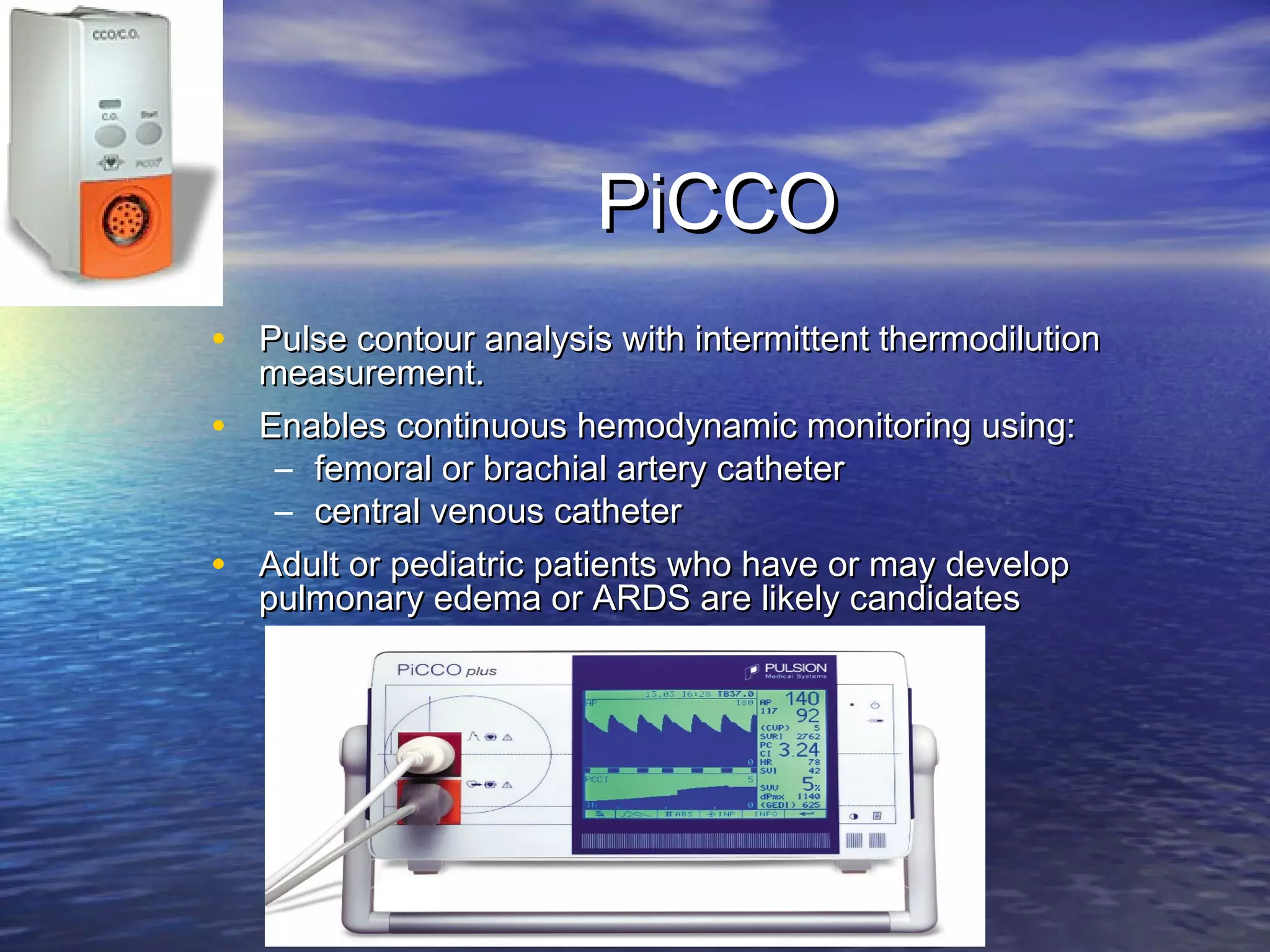
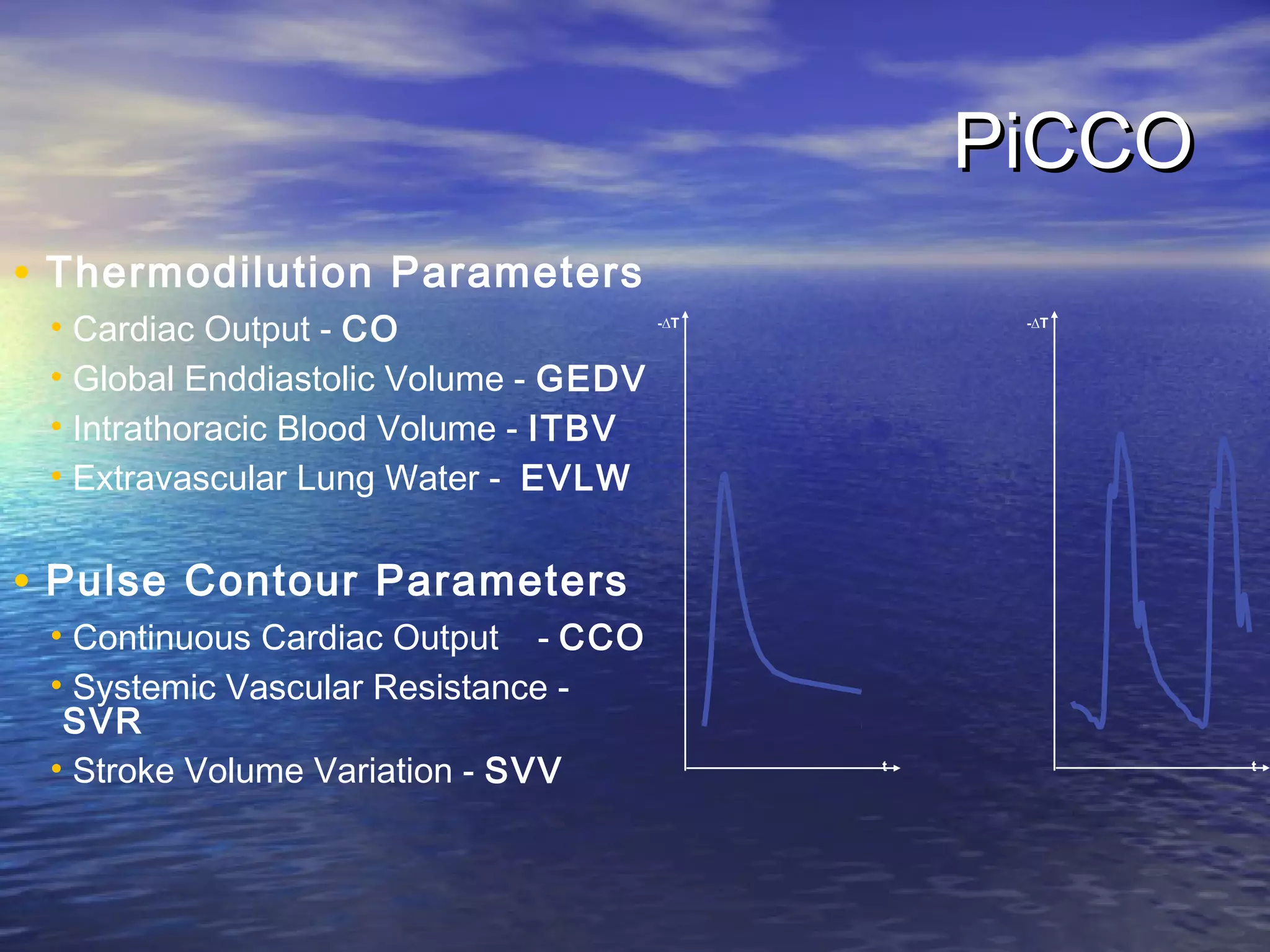
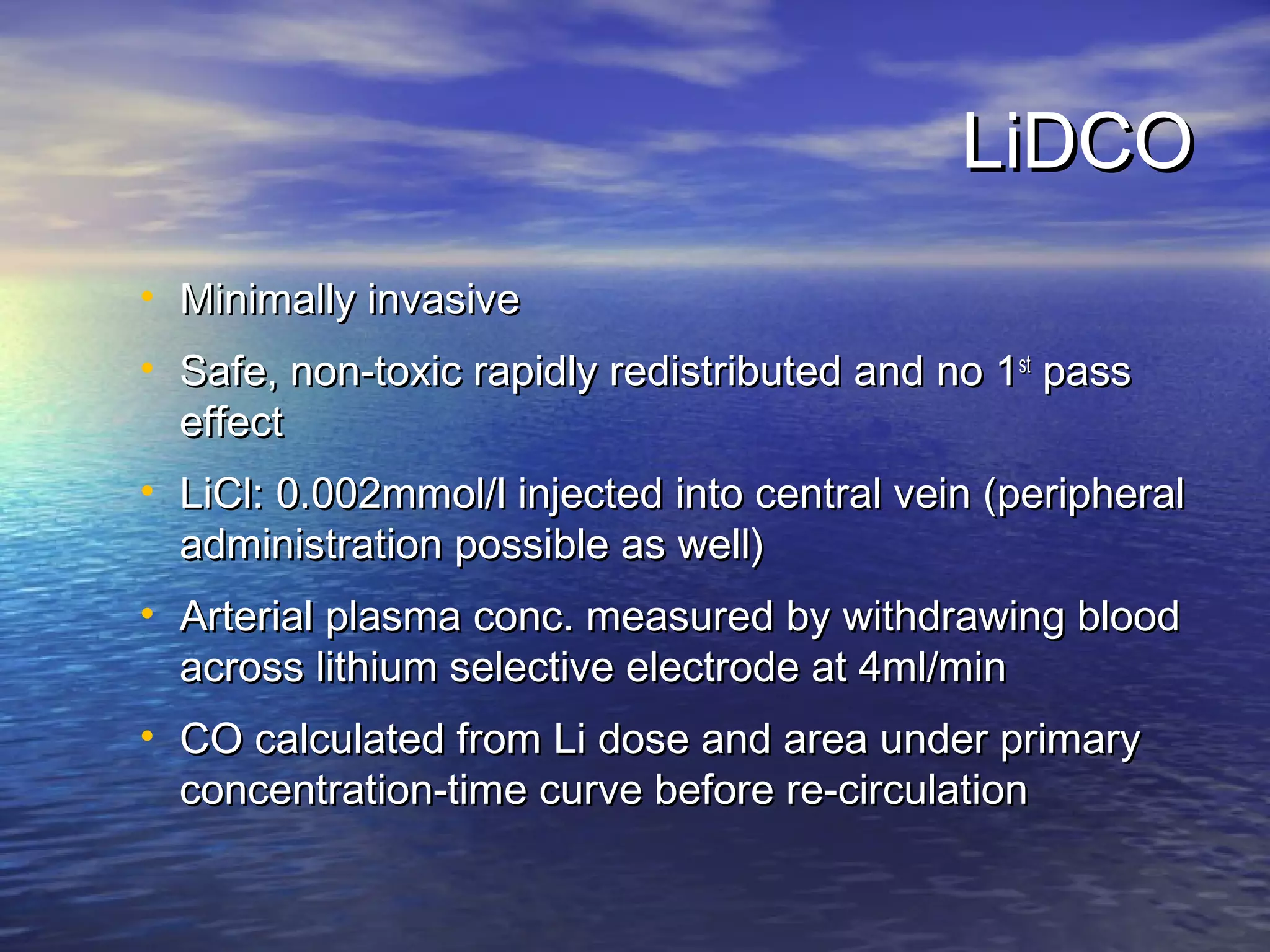
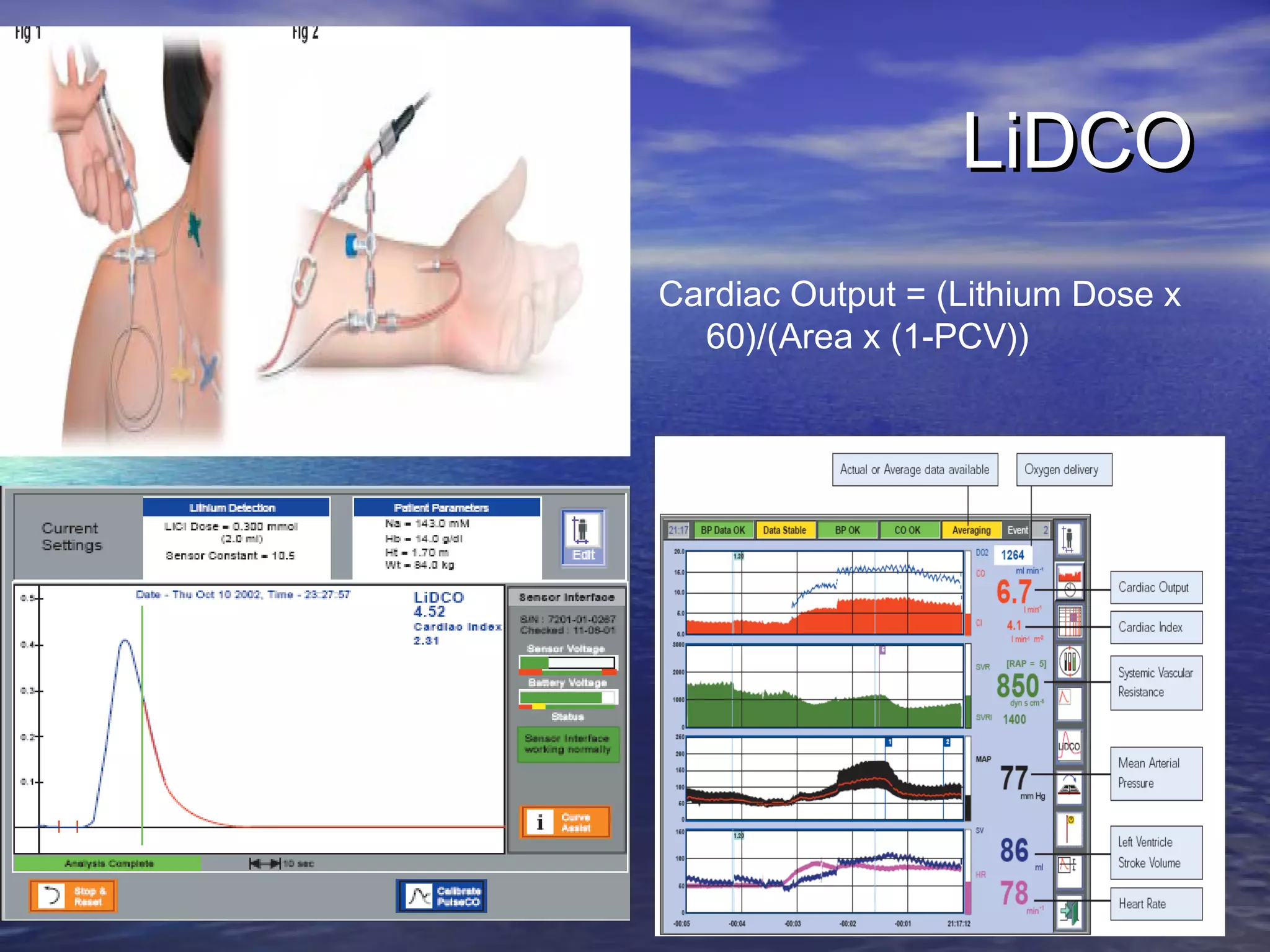
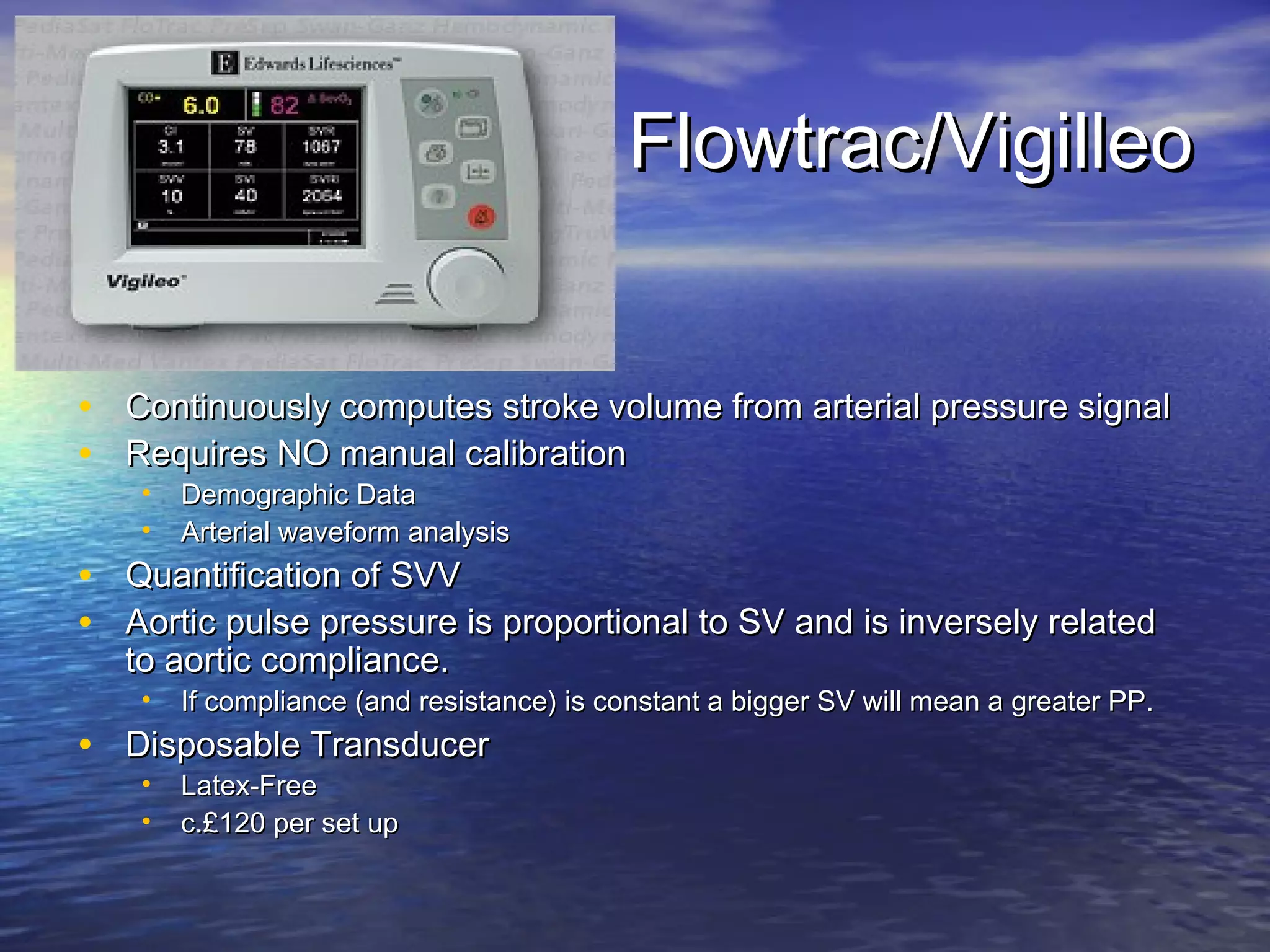
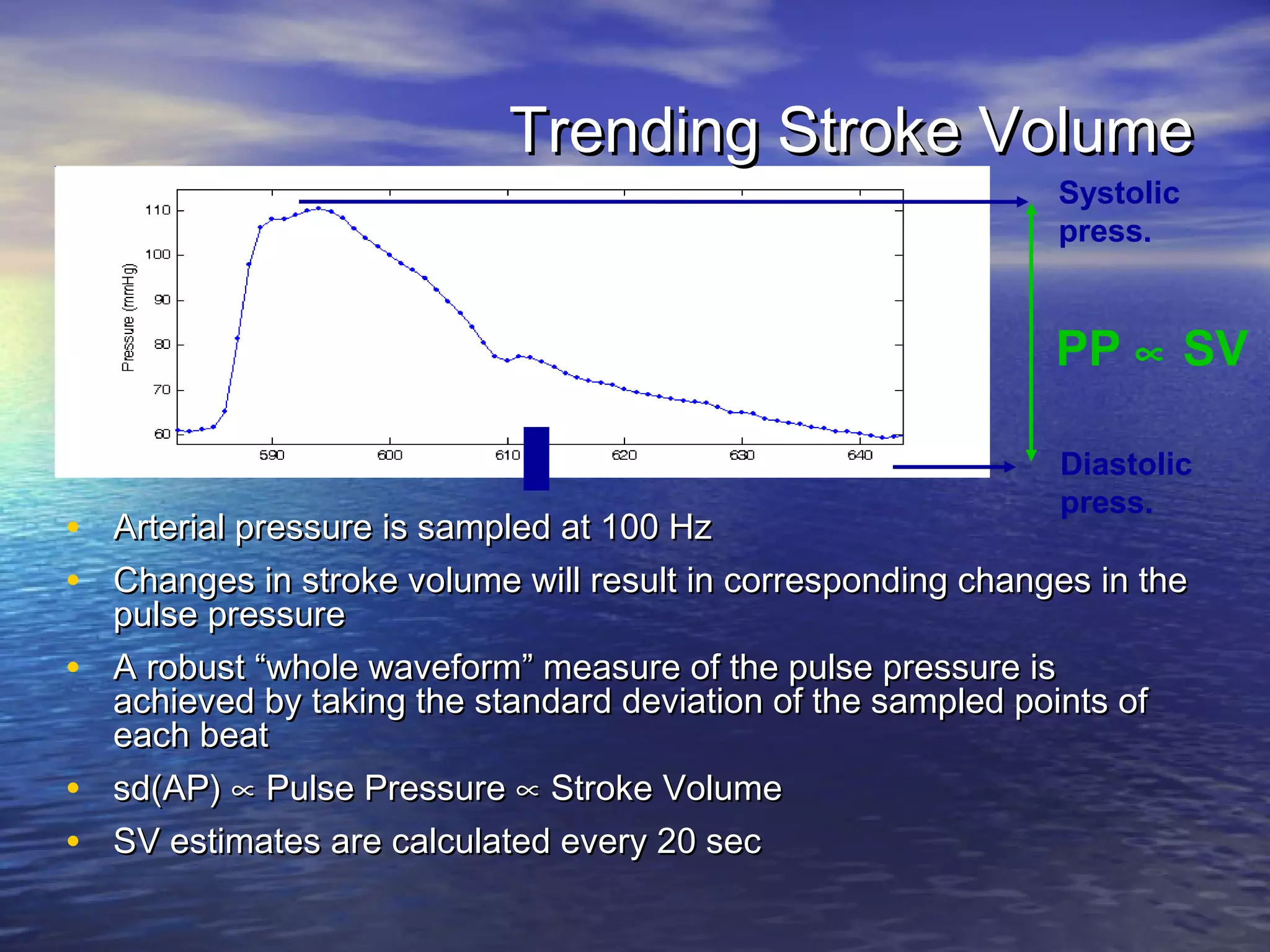
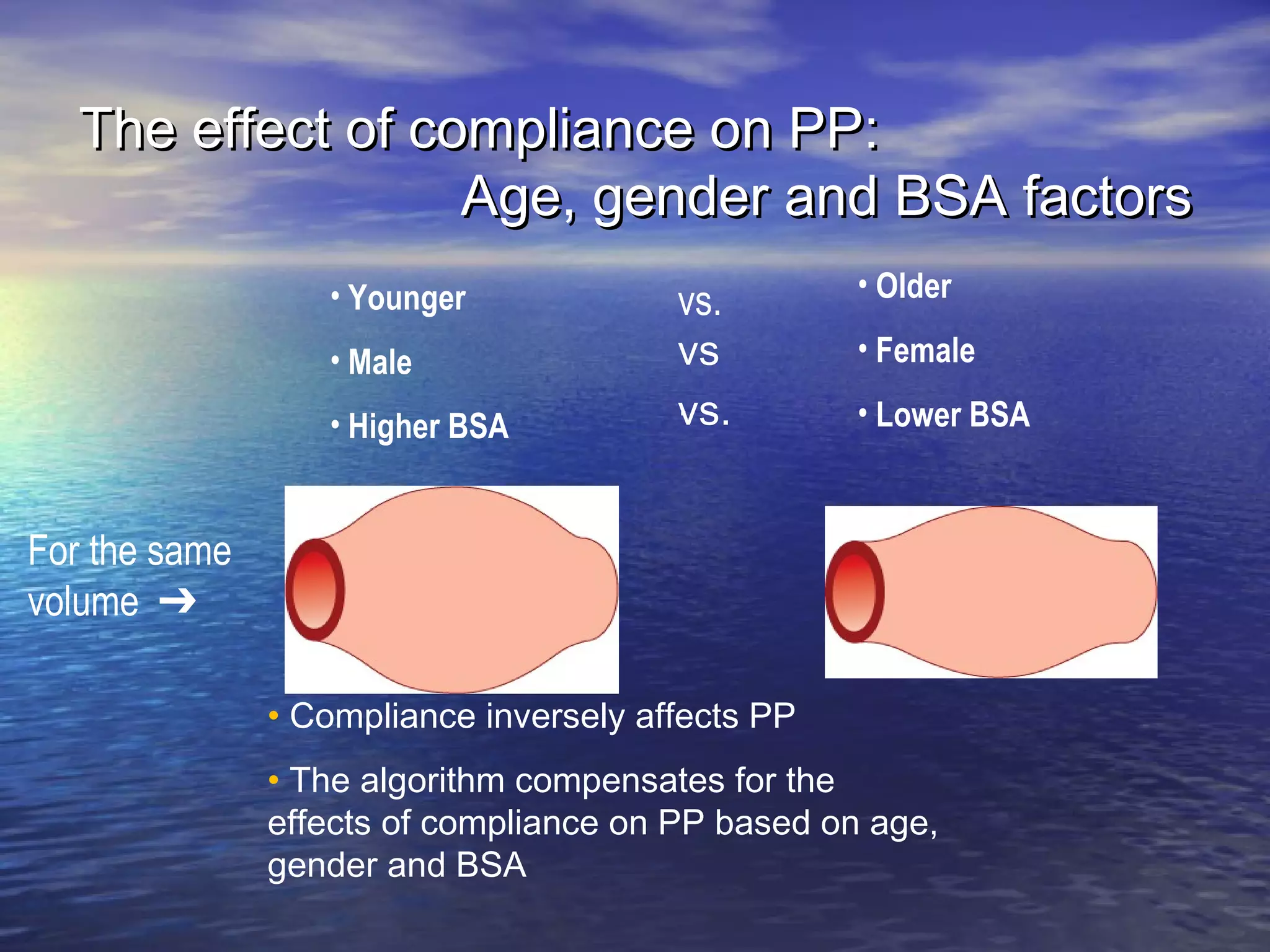
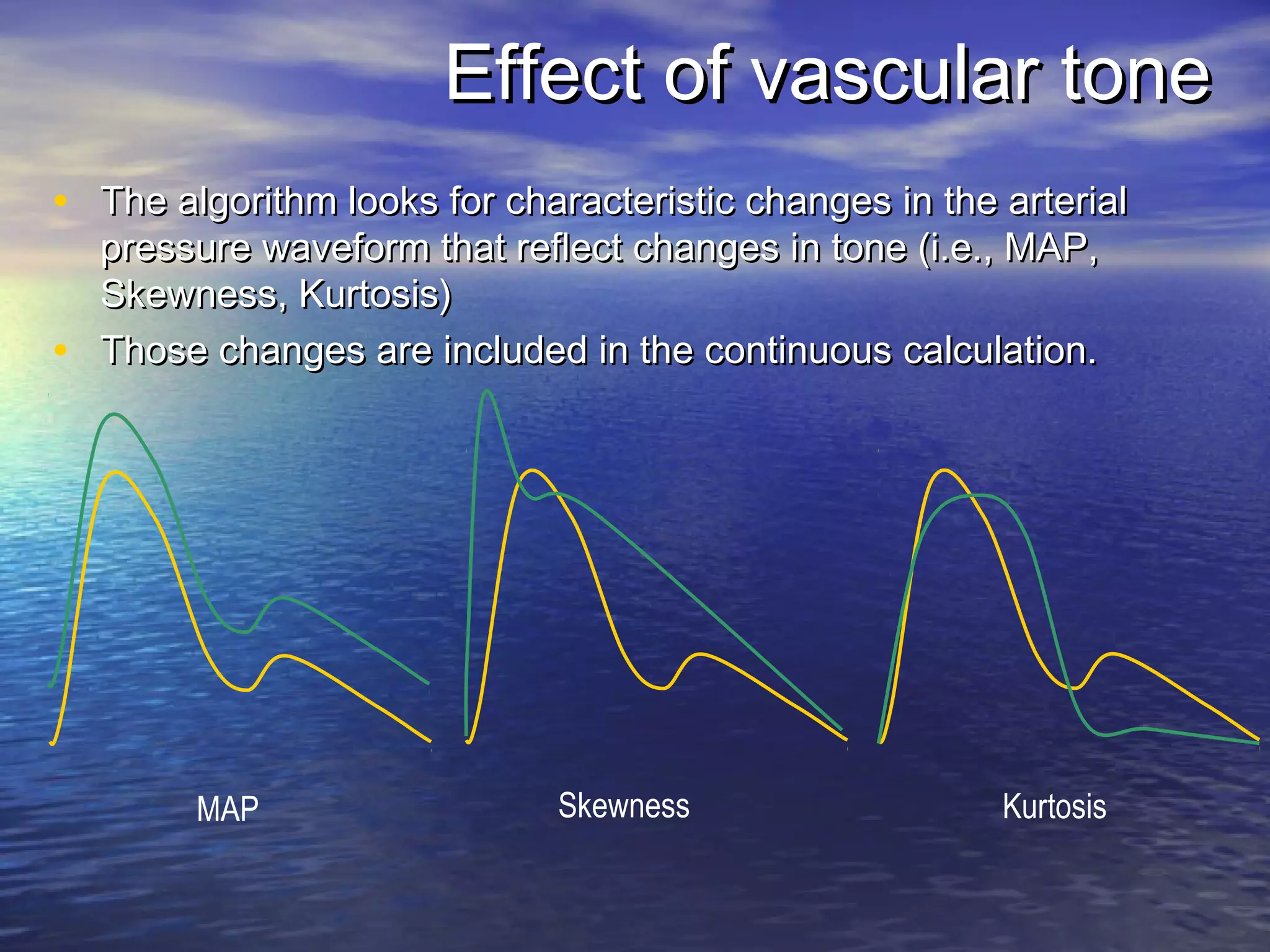
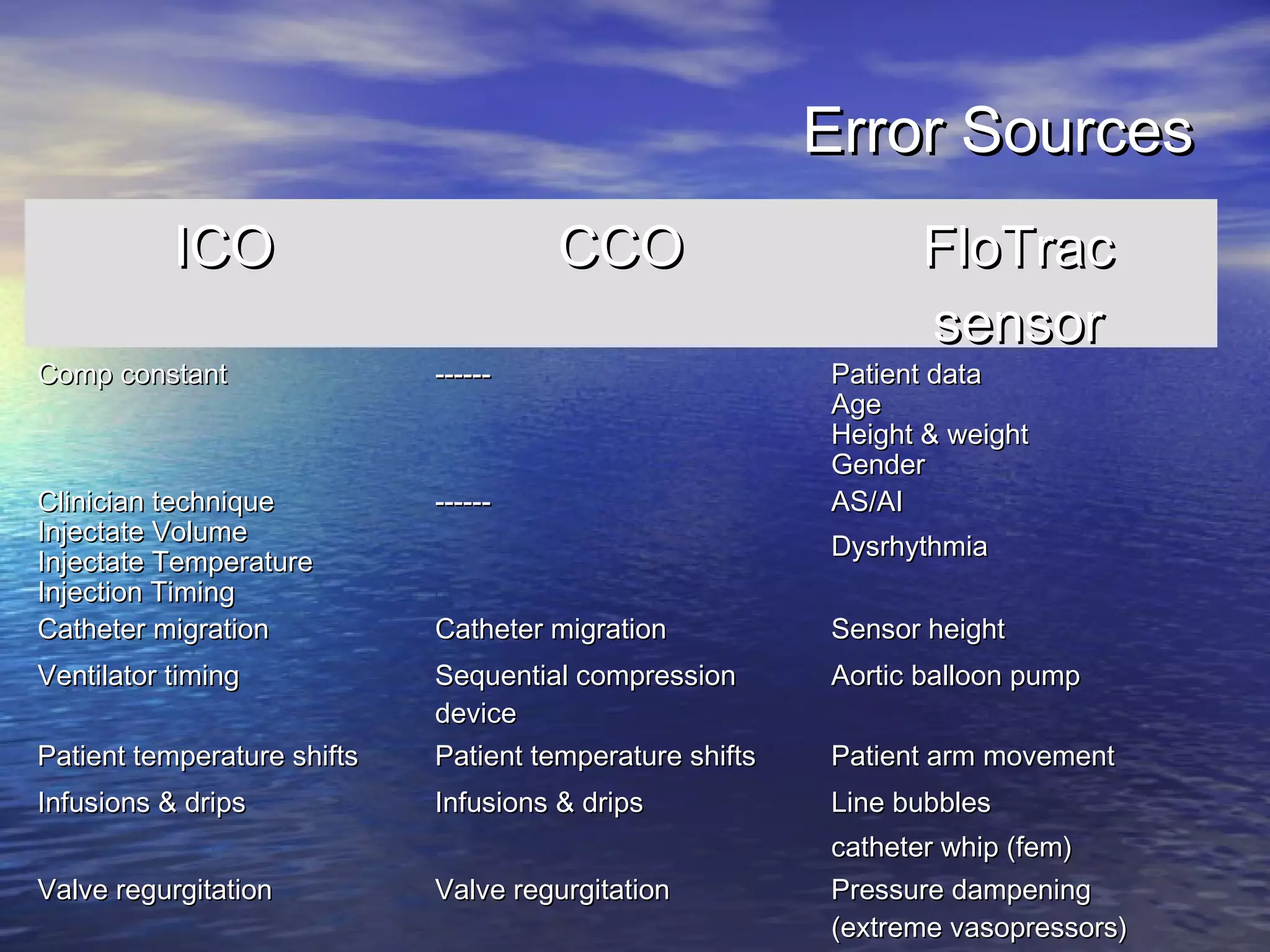
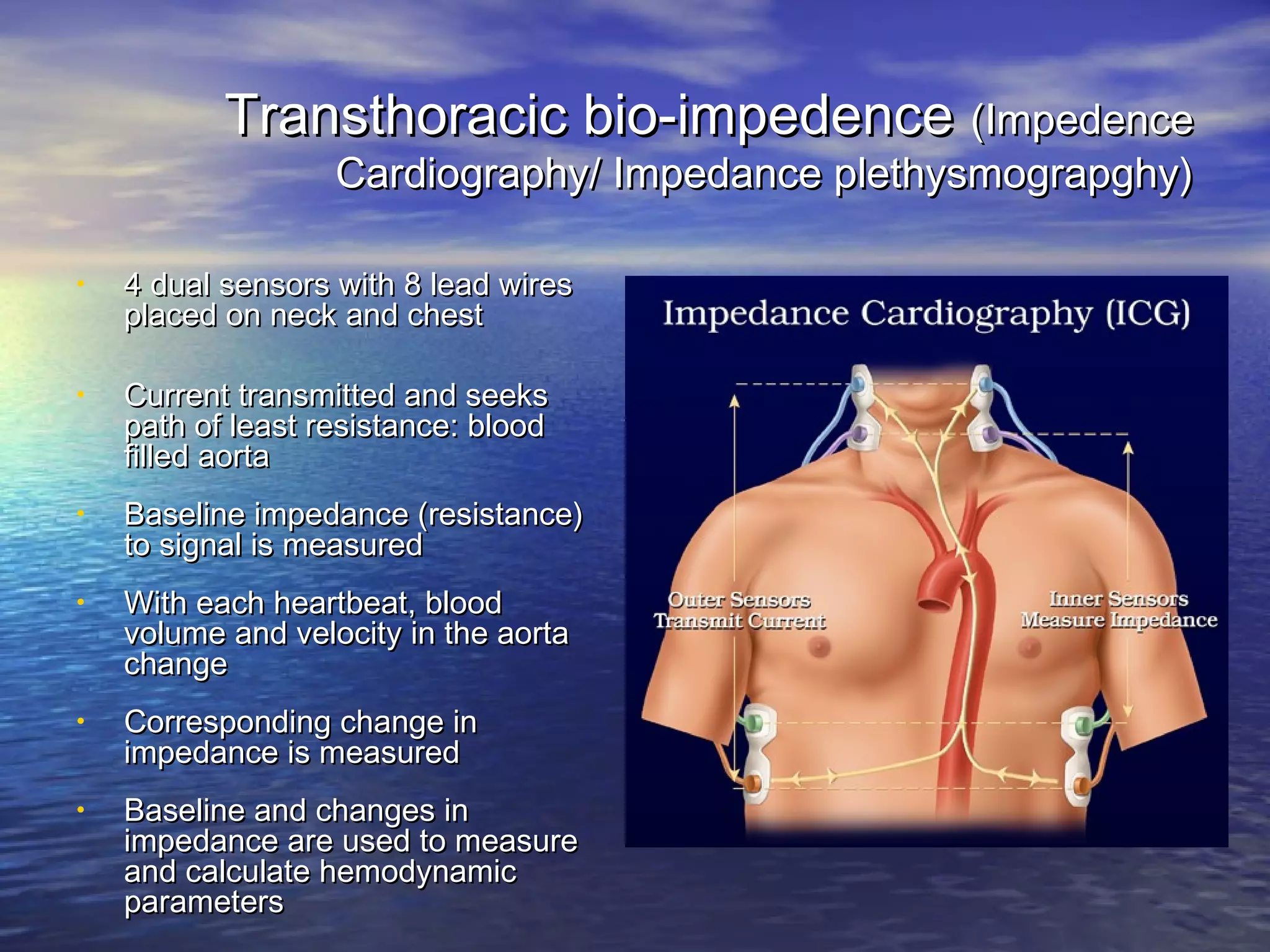
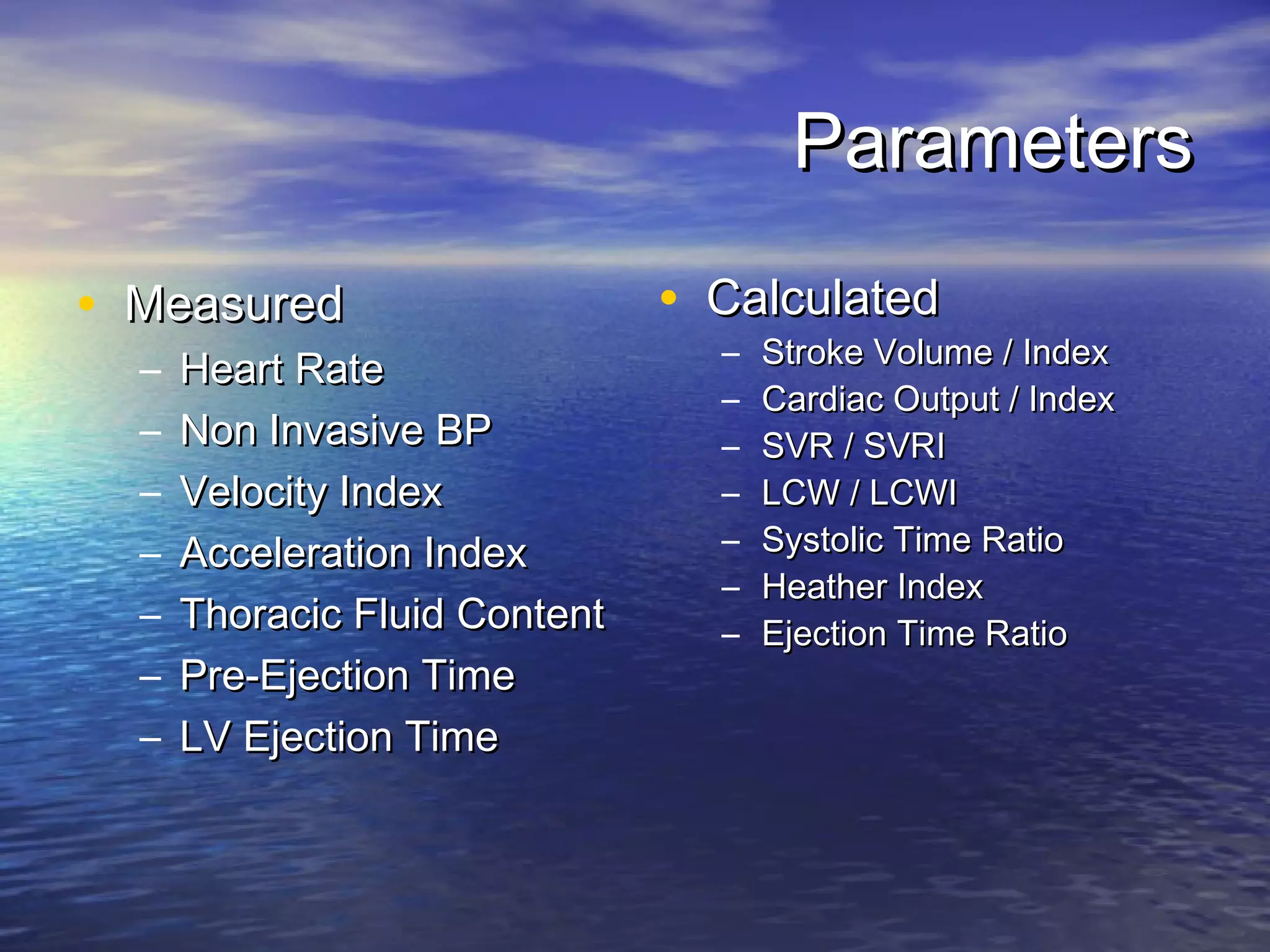
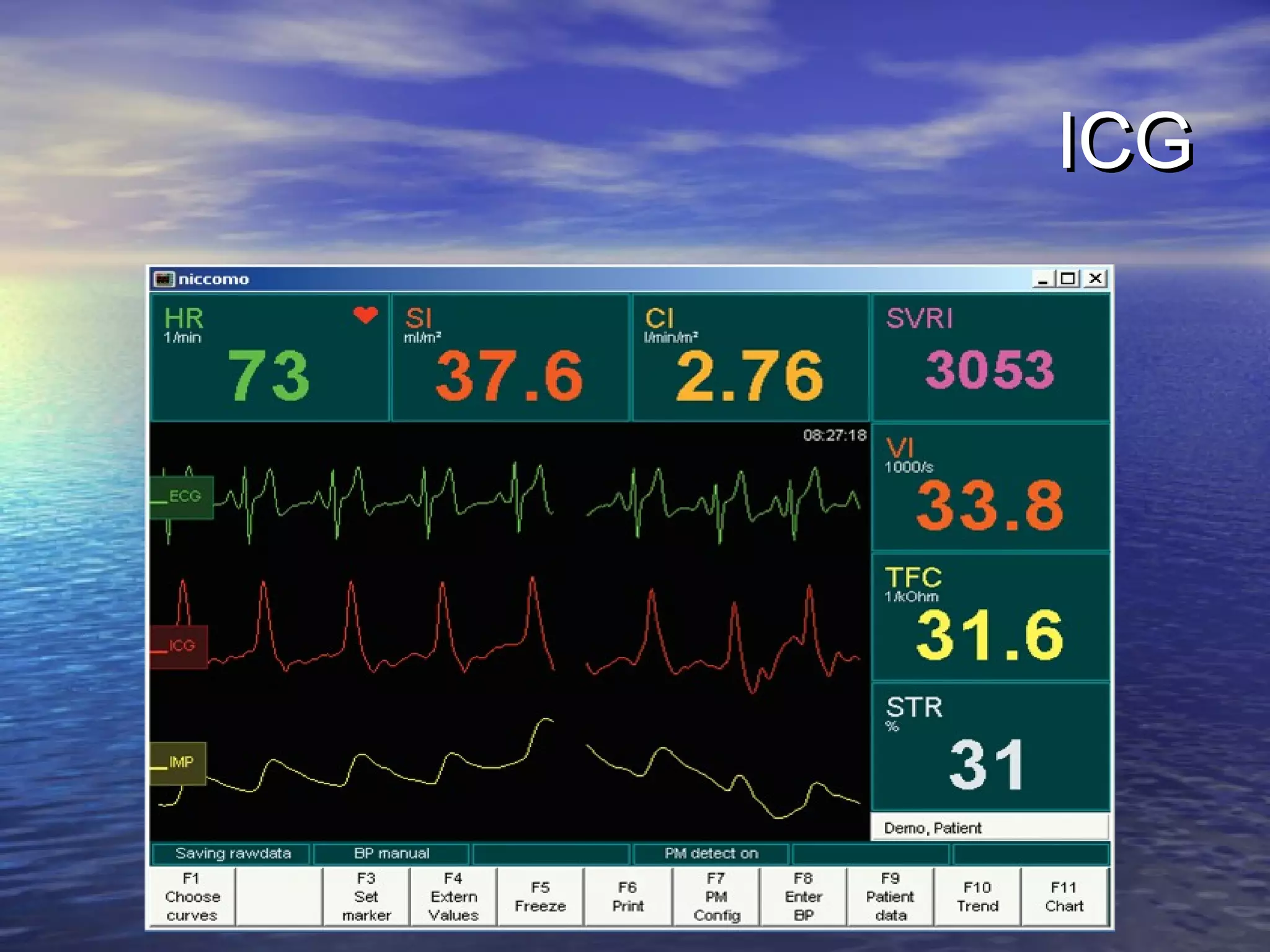
This document discusses various techniques for monitoring cardiac output (CO), including invasive and non-invasive options. It provides details on pulmonary artery catheters, the Fick principle, transesophageal echocardiography, esophageal Doppler, pulse contour analysis methods (PiCCO, LiDCO, Flowtrac), transthoracic bioimpedance, and transthoracic echocardiography. While some methods like pulmonary artery catheters and LiDCO are well-validated, the document notes that rigorous validation studies are still needed for newer non-invasive options like Flowtrac and transthoracic bioimpedance. Overall, it emphasizes understanding the limitations of different CO monitoring systems and using trends over